This is EM Cases Episode 92 – PALS Guidelines.
I remember when I started practicing emergency medicine a decade and a half ago it seemed that any kid who came to our ED in cardiac arrest died. I know, depressing thought. But, over the past 15 years, survival to discharge from pediatric cardiac arrest has markedly improved, at least for in-hospital arrests. This is probably mostly due to an emphasis on high-quality CPR and advances in post-resuscitation care; nonetheless the more comfortable, knowledgeable and prepared we are for the always scary critically ill pediatric patient, the more likely we will be able to resuscitate them successfully – which is always a huge save.
With this mission in mind Dr. Allan DeCaen, a pediatric intensivist at Stollery in Edmonton and the director of the pediatric ICU transport team, as well as the writing group chair for the American heart association and heart and stroke Canada PALS guidelines, and Dr. Anthony Crocco division head and medical director of the pediatric emergency program at McMaster children’s hospital, will walk us through highlights from the recent AHA PALS guidelines including:
- How to recognize pediatric shock and prevent cardiac arrest before it’s too late
- Key differences in pediatric anatomy and physiology to help guide management
- How to maximize effective CPR
- The indications for atropine and antidysrhythmics in children
- How to improve post-cardiac arrest care in children
Podcast produced by Anton Helman, voice editing by Richard Hoang,
sound design by Anton Helman
Written Summary and blog post written by Michael Kilian, edited by Anton Helman March, 2017
Cite this podcast as: Helman, A, DeCaen, A, Crocco, A. PALS Guidelines. Emergency Medicine Cases. March, 2017. https://emergencymedicinecases.com/uti-myths-misconceptions/. Accessed [date].
It’s best to avoid cardiac arrest in the first place: Early identification of shock
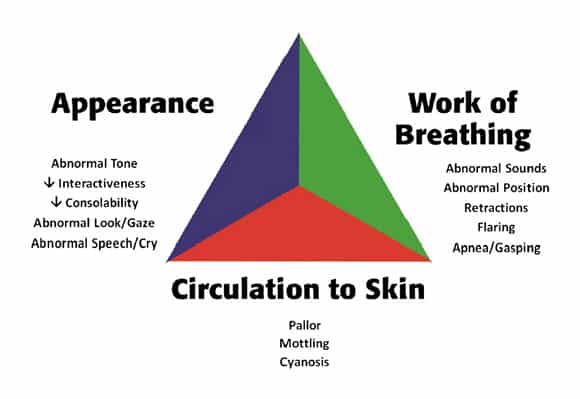
The pediatric assessment triangle, provides a valuable checklist that we should go through for every child we see in the ED to help us assess their risk of crashing. The pediatric assessment triangle is based solely on observing the child from the foot of the bed.
Pediatric assessment triangle
The Pediatric Early Warning Score (PEWS) isn’t good enough
There is little evidence that the use of PEWS (tool that is based on 5 domains: behavior, cardiovascular status, respiratory status, nebulizer use, and persistent vomiting) outside of the pediatric ICU setting reduces hospital mortality. In one observational study, PEWS use was associated with a reduction in cardiac arrest rate when used in a single hospital with an established medical emergency team system.
The importance of accurate interpretation of heart rate and respiratory rate in early identification of pediatric shock
One of the main reasons that we sometimes tend to under-recognize the deteriorating child is because their blood pressure often remains normal until they suddenly crash and arrest. Because of their high sympathetic tone, children can maintain a seemingly normal blood pressure longer than an adultwould, making hypotension a very late finding in a critically ill child. This can make early recognition of sepsis more challenging in children. The keys to early identification of pediatric sepsis lies in the heart rate and respiratory rate, both of which will increase disproportionately to the fever in sepsis. We must consider tachycardia an early warning sign for sepsis. While individual vital signs are sensitive but not specific, multiple abnormal vital signs taken together have an improve specificity for sepsis.
Assessing whether or not a child is tachycardic and tachypneic is vital in weighing your suspicion for shock. The acceptable upper limit of heart rate changes as children get older. A number of resources have published ranges of acceptable heart and respiratory rates for different age groups. A commonly used resource is the PALS guidelines. In 2011, Fleming et al. published a systematic review in The Lancet, describing normal heart and respiratory rate for children based on existing published data. They compared their findings with the PALS ranges and found that PALS ranges were higher than both the median and 90th percentiles obtained in the systematic review. Our experts advocate using the more conservative values from the systematic review when evaluating a child for signs of shock.

Pediatric Vital Signs Pocket Card listing the 90th percentile cut-offs for heart rate and respiratory rate
Download pdf of this pocket card HERE.
If you over call shock, that’s okay. Be conservative when it comes to identifying shock in children. If you think it might be shock, but you aren’t sure, start resuscitating on speculation.
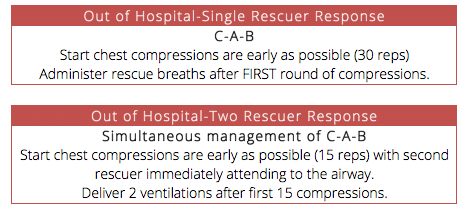
C-A-B vs. A-B-C Approach in PALS: Chest compression only CPR is not advisable in pediatric cardiac arrest
The C-A-B approach has been advocated in adult cardiac arrest with the goal of starting chest compressions as early as possible and minimizing interruptions. However, adult arrests are usually cardiac related, whereas children tend to arrest from respiratory causes which tend to be mediated by hypoxia. Our experts advocate the following approaches to pediatric cardiac arrests:
Chest compression-only CPR in the field is not advisable in kids as it is in adults. You need to be starting breaths by the end of the first cycle of chest compressions at the 16 second mark. The asphyxial nature of the majority of pediatric cardiac arrests necessitates ventilation as part of effective CPR, and 2 large database studies documented worse 30-day outcomes with compression-only CPR compared with conventional CPR. For this reason, conventional CPR (chest compressions and rescue breaths) is a Class I recommendation (LOE B-NR) for children.
For in-hospital arrests addressing airway, breathing and circulation – i.e. ensuring a patent airway, oxygenation and chest compressions should all start simultaneously.
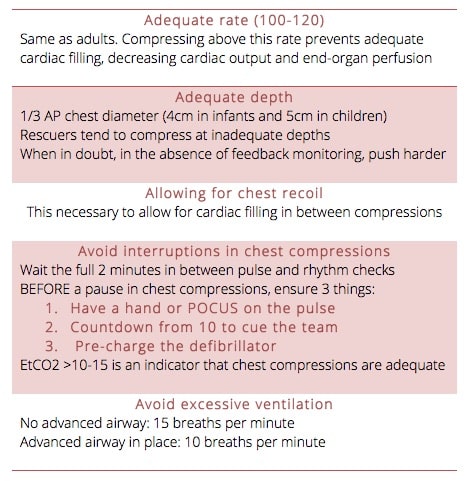
The 5 components of good CPR in PALS
Monitoring and ensuring high quality of CPR:
Our experts recommend the following strategies in order to ensure high quality CPR during a resuscitation:
- EtCO2: High quality CPR will produce EtC02 of 10-15 mmh Hg as a marker of good pulmonary blood flow and cardiac output.
- Using pads with accelerometers that monitor both the rate of compressions and depth of compressions and provide audio-feedback: “press harder, press faster”.
- Handover responsibility to a team member to monitor the quality of CPR during the resuscitation and provide feedback on ventilation and compressions.
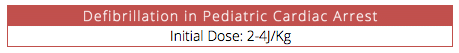
Defibrillation in PALS Guidelines
The initial dose for defibrillation in kids is 2-4J/kg and it’s not unreasonable to go higher if necessary according to our experts.
Lidocaine is added to to the PALS guidelines in the cardiac arrest algorithm for shock resistant VF and pVT
New pediatric observational data from 2015 by Valdes et. al shows that lidocaine is associated with increased likelihood for ROSC compared to amiodarone. Although there was a benefit in short term outcomes, there was no association between use of either drug and survival to hospital discharge. For patients who are in shock-refractory VF or pVT, either lidocaine or amiodarone may be used.
Airway considerations: larger tongues, anterior cords and larger occiputs
There are number of anatomical differences to be aware of when resuscitating a child compared to an adult. Beginning with the airway, children have larger tongues, making them more prone to obstruction with altered GCS or sedating medications. Children also have much more anterior vocal cords compared to adults. Their larger occiputs make it challenging to obtain an adequate view of their anterior structures during intubation. To overcome these anatomical challenges, position the patient with a shoulder roll to extend the neck.
Update 2022: An observational study using data from 2 national airway consortiums including 1,412 emergency pediatric intubations found that video-assisted laryngoscopy was associated with higher odds of first-attempt success (OR 2.01) and 30% reduced odds of experiencing severe adverse airway outcomes. Abstract

Large occiput contributes to neck flexion in the supine position and more difficult access to anterior airway

A shoulder roll helps extend the neck and compensate for the larger occiput
Atropine pre-treatment for RSI: Not routine in PALS Guidelines
When it comes to pretreatment drugs for RSI in critically ill children, atropine at 0.02mg/kg 3-5 minutes prior to sedative and paralytic drugs for RSI should not be given routinely.
Recent observational data comparing the use of atropine vs. no atropine in the intubation of critically ill children suggests that there might be some benefit to using atropine.
Consider the use Atropine (0.02mg/kg) prior to RSI for patients at risk of severe bradycardia:
- <1 year of age
- Succinylcholine
- If the patient is already bradycardic
There is no role for atropine in a patient who is in cardiac arrest.
Pediatric Septic Shock: Update in fluid management and vasoactive medication of choice
Be mindful of fluid overload in pediatric septic shock
Traditionally it has been suggested that children suffering from septic shock receive 20mL/kg IV or IO bolus NS, repeated twice to total of 60mL/kg. This was discussed in details in the EM Cases episode Recognition and Management of Pediatric Sepsis and Septic Shock.
Two studies have challenged the notion of early aggressive fluid therapy in pediatric septic shock:
- The FEAST Trial Group from NEJM 2011 studied children with signs of shock and fever in sub saharan Africa which showed that bolus therapy of NS or albumin was associated with greater mortality risk.
- Van paridon et al from Critical Care 2015 suggest that the amount of fluid given during resuscitation is associated with longer ICU stays and longer time on a ventilator.
In light of these studies, our experts advocate to continue with the 20cc/kg bolus approach but be sure to reassess patients often, monitoring for signs of hypervolemia, and consider early use of ionotropes such as epinephrine.
Epinephrine is the vasoactive medication of choice for pediatric septic shock
Given that children most commonly present in cold shock (as apposed to warm shock as in adultsas discussed on the EM Cases episode on pediatric sepsis and septic shock), our experts advocate epinephrine as the first vasoactive medication of choice. This is a departure from earlier dogma which considered dopamine to be the first line vasopressor of choice. The use of epinephrine is supported by a double-blind, prospective control trial comparing epinephrine and dopamine, which showed that dopamine was associated with increased risk of death and healthcare associated infections.
Consideration for ECMO and cardiopulmonary bypass in PALS
There are no validated published indications for pediatric ECMO and the decision to start ECMO post arrest should be done on a case by case basis in consultation with a pediatric intensivist.
Make the call early!
Our experts suggest that 5 minutes into the resuscitation of a cardiac arrest pediatric patient is an appropriate time to call your pediatric intensivist to consider ECMO.
While there are few ECMO centers in Canada, there are an increasing number of cannulation programs where the process is started at the base hospital and the patient is transferred to an ECMO centre.
PALS Post Arrest Care
Targeted temperature management: Avoid fever!
There is little evidence to suggests that hypothermia (32-34 C) is superior to normothermia (36-37C). Our experts agree with the PALS guidelines that the most important aspect of post cardiac arrest temperature management is to prevent hyperthermia.
Update 2017: Since the recording of this podcast, Moler et al published a trial in the NEJM comparing therapeutic hypothermia (target temp 33 Cel) to targeted temperature management (target temp 36.8 Cel). The study was stopped early because no difference was seen in one year survival or functional outcomes. This confirms no superiority for hypothermia and reinforces the need to avoid hyperthermia.
Dr. DeCaen, Dr. Crocco, Dr. Helman and Dr. Kilian have no conflicts of interest to declare
For more EM Cases content on Pediatric Emergencies check out our free interactive eBook,
EM Cases Digest Vol. 2 Pediatric Emergencies here.
For more Pediatric EM learning visit one of EM Cases collaborators trekk.ca – Translating Emergency Knowledge for Kids (TREKK) is a growing network of researchers, clinicians, health consumers and national organizations who want to accelerate the speed at which the latest knowledge in children’s emergency care is put into practice in general EDs – rural, remote or urban.
References
Seiger N, Maconochie I, Oostenbrink R, Moll HA. Validity of different pediatric early warning scores in the emergency department. Pediatrics. 2013;132(4):e841-50.
Fleming S, Thompson M, Stevens R, et al. Normal ranges of heart rate and respiratory rate in children from birth to 18 years of age: a systematic review of observational studies. Lancet. 2011;377(9770):1011-8.
Van paridon BM, Sheppard C, G GG, Joffe AR. Timing of antibiotics, volume, and vasoactive infusions in children with sepsis admitted to intensive care. Crit Care. 2015;19:293.
Neumar RW, Shuster M, Callaway CW, et al. Part 1: Executive Summary: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132(18 Suppl 2):S315-67.
Atkins DL, Berger S, Duff JP, et al. Part 11: Pediatric Basic Life Support and Cardiopulmonary Resuscitation Quality: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132(18 Suppl 2):S519-25.
De caen AR, Berg MD, Chameides L, et al. Part 12: Pediatric Advanced Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132(18 Suppl 2):S526-42.
Marsch S, et al. ABC versus CAB for cardiopulmonary resuscitation: a prospective, randomized simulator-based trial. Swiss Med Wkly. 2013;143:w13856. doi: 10.4414/ smw.2013.13856.
Sekiguchi H, Kondo Y, Kukita I. Verification of changes in the time taken to initiate chest compressions according to modified basic life support guidelines. Am J Emerg Med. 2013;31:1248–1250. doi: 10.1016/j.ajem.2013.02.047.
Lubrano R, et al. Comparison of times of intervention during pediatric CPR maneuvers using ABC and CAB sequences: a randomized trial. Resus
Sutton RM, et al. Pushing harder, pushing faster, minimizing interruptions… but falling short of 2010 cardiopulmonary resuscitation targets during in-hospital pediatric and adolescent resuscitation. Resuscitation. 2013;84:1680–1684.
Sutton RM, et al. 2010 American Heart Association recommended compression depths during pediatric in-hospital resuscitations are associated with survival. Resuscitation. 2014;85:1179–1184.
Kitamura T, et al. Implementation working group for All-Japan Utstein Registry of the Fire and Disaster Management Agency. Conventional and chest-compression-only cardiopulmonary resuscitation by bystanders for children who have out-of-hospital cardiac arrests: a prospective, nationwide, population-based cohort study. Lancet. 2010;375:1347–1354.
Goto Y, Maeda T, Goto Y. Impact of dispatcher-assisted bystander cardiopulmonary resuscitation on neurological outcomes in children with out-of hospital cardiac arrests: a prospective, nationwide, population-based cohort study. J Am Heart Assoc. 2014;3:e000499.
Randhawa S, Roberts-Turner R, Woronick K, DuVal J. Implementing and sustaining evidence-based nursing practice to reduce pediatric cardiopulmonary arrest. West J Nurs Res. 2011;33:443–456.
Maitland K, et al. FEAST Trial Group. Mortality after fluid bolus in African children with severe infection. N Engl J Med. 2011;364:2483–2495.
Upadhyay M, et al. Randomized evaluation of fluid resuscitation with crystalloid (saline) and colloid (polymer from degraded gelatin in saline) in pediatric septic shock. Indian Pediatr. 2005;42:223–231.
Jones P, et al. Atropine for critical care intubation in a cohort of 264 children and reduced mortality unrelated to effects on bradycardia. PLoS One. 2013;8:e57478.
Jones P, et al. The effect of atropine on rhythm and conduction disturbances during 322 critical care intubations. Pediatr Crit Care Med. 2013;14:e289– e297.
Fastle RK, Roback MG. Pediatric rapid sequence intubation: incidence of reflex bradycardia and effects of pretreatment with atropine. Pediatr Emerg Care. 2004;20:651–655.
Valdes SO, et al. American Heart Association Get With The GuidelinesResuscitation Investigators. Outcomes associated with amiodarone and lidocaine in the treatment of in-hospital pediatric cardiac arrest with pulseless ventricular tachycardia or ventricular fibrillation. Resuscitation. 2014;85:381–386.
Ventura AM, Shieh HH, Bousso A, et al. Double-Blind Prospective Randomized Controlled Trial of Dopamine Versus Epinephrine as First-Line Vasoactive Drugs in Pediatric Septic Shock. Crit Care Med. 2015;43(11):2292-302.
Moler FW, Silverstein FS, Holubkov R, et al. Therapeutic Hypothermia after In-Hospital Cardiac Arrest in Children. N Engl J Med. 2017;376(4):318-329.
Other FOAMed Resources on Pediatric Cardiac Arrest Care
PEMBlOG on AHA/PALS Medication Updates
PulmCC on therapeutic hypothermia in kids
Now test your knowledge with a quiz.





Wonderful and thorough discussion of resuscitation in pediatrics!
There seems to be a discrepancy between this episode and Episode 50 Recognition and Management of Pediatric Sepsis and Septic Shock with regards to vasopressors. If I have understood correctly you recommend using epinephrine as the vasoactive medication of choice for pediatric septic shock in episode 93, but in Episode 50 you recommend Dopamine as the first choice of pressors and THEN IF:
1.Cold Shock: Epinephrine
2.Warm Shock: Norepinephrine ..
Can you pleas clarify this?
Since Episode 50 there has been a move away from Dopamine and so the latest guidelines suggest Epinephrine as the first line. The vast majority of kids will present in cold shock and so epinephrine is first line in most cases. For older patients who present in warm shock like adults, norepinephrine is first line.