Resuscitation
Best Case Ever 7: Atrial Fibrillation
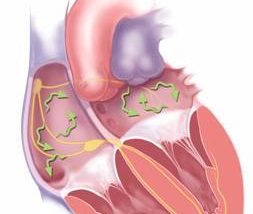
As a bonus to Episode 20 on Atrial Fibrillation, we present here, Dr. Clare Atzema, a leading EM researcher in Atrial Fibrillation, telling her Best Case Ever related to Afib. What would you do if you needed to cardiovert a patient who was too obese to fit on an ED stretcher? Dr. Atzema, along with Dr. Nazanin Meshkat and Dr. Bryan Au, discuss the presentation, etiology, precipitants, management and disposition of Atrial Fibrillation in the Emergency Department. The pros and cons of rate vs rhythm control are debated, what you need to know about Afib medications, and the value of the Ottawa Aggressive Protocol discussed. The importance of appropriate anticoagulation is detailed, with a review of the CHADS-VASc score and whether to use anticogulants or ASA for stroke prevention for patients with Afib. We end off with a discussion on how to recognize and treat Wolff-Parkinson-White syndrome in the setting of Atrial Fibrillation. [wpfilebase tag=file id=382 tpl=emc-play /] [wpfilebase tag=file id=383 tpl=emc-mp3 /]
Episode 18 Part 1: Point of Care Ultrasound Pearls, Pitfalls and Controversies
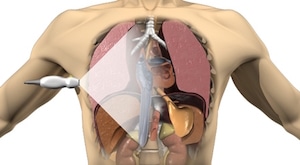
In this first installment of this Episode, Point of Care Ultrasound Pearls, Pitfalls & Controversies we have a panel of POCUS gurus, Dr. Greg Hall, Dr. Jordan Chenkin, Dr. Paul Hannam & Dr. Jason Fischer. They review the basic criteria for commonly used, practical Point of Care Ultrasound indications at the bedside and then dive into heated debate about specific pearls and pitfalls in Point of Care Ultrasound assessment of the patient with undifferentiated shortness of breath, undifferentiated shock, cardiac arrest and swollen leg. They discuss how best to interpret the massive body of literature for POCUS and when we can hang our hats on our Point of Care Ultrasound findings.
Episode 15 Part 2: Acute Coronary Syndromes Management
In Part 2 of this Episode on Acute Coronary Syndromes Risk Stratification & Management, the evidence for various medications for ACS, from supplemental oxygen to thrombolytics are debated, and decision making around reperfusion therapy for STEMI as well as NSTEMI are discussed. Finally, there is a discussion on risk stratification of low risk chest pain patients and all it's attendant challenges as well as disposition and follow-up decisions. Dr. Eric Letovsky, the Head of the CCFP(EM) Program at the University of Toronto, Dr. Mark Mensour & Dr. Neil Fam, an interventional cardiologist answer questions like: What is the danger of high flow oxygen in the setting of ACS? When, if ever, should we be using IV B-blockers in AMI patients? How can you predict, in the ED, who might go on to have an urgent CABG, in which case Clopidogrel is contra-indicated? Which anticoagulant is best for unstable angina, NSTEMI and STEMI - unfractionated heparin (UFH), low molecular weight heparin (LMWH), or fonduparinux? Is there currenly any role for Glycoprotein 2b3a Inhibitors in ACS in the ED? When is thrombolysis better than PCI for STEMI? When should we consider facilitated angioplasty and rescue angioplasty? Which low risk chest pain patients require an early stress test? CT coronary angiography? Stress Echo? Admission to a Coronary Decision Unit (CDU)? and many more.......
Episode 12 Part 2: ACLS Guidelines – Atropine, Adenosine & Therapeutic Hypothermia
In Part 2 of this episode on ACLS Guidelines - Atropine, Adenosine & Therapeutic Hypothermia, Dr. Steven Brooks and Dr. Michael Feldman discuss the removal of Atropine from the PEA/Asystole algorithm, the indications and dangers of Adenosine in wide-complex tachycardias, pressors as a bridge to transvenous pacing in unstable bradycardias, and the key elements of post cardiac arrest care including therapeutic hypothermia and PCI. They answer questions such as: In which arrhythmias can Amiodarone cause more harm than good? Is there any role for transcutaneous pacing for asystole? When should Bicarb be given in the arrest situation? In what situations is Atropine contra-indicated or the dosage need to be adjusted? How has the widespread use of therapeutic hypothermia currently effected our ability to prognosticate post-arrest patients? What are the indications for PCI and thrombolysis in the cardiac arrest patient? Should we be using therapeutic hypothermia in the non-Vfib arrest patient? What is the best method for achieving the target temperature for the patient undergoing therapeutic hypothermia? and many more......
Episode 12 Part 1: ACLS Guidelines – What’s New & Controversial
In Part 1 of this episode on the latest ACLS Guidelines, Dr. Steven Brooks and Dr. Michael Feldman review and debate what's new and what's controversial in the the 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Within the frameworks of Cardiocerebral Rescusitation and the 3 phase model of rescucitation (electrical, circulatory and metabolic), they discuss the importance of high quality CPR, the de-emphasis on early ventilation and the utility of continuous quantitative waveform capnography. Dr. Brooks and Dr. Feldman answer questions such as: of all the therapeutic manoeuvres we do for the cardiac arrest patient, which ones have been shown to improve survival to hospital discharge? What is the evidence for chest compression machines? What is the utility of bedside ultrasound in the cardiac arrest patient? Why is cardiac arrest survival to discharge in Seattle the best in the world? Should we be performing 'hands-on defibrillation'? and many more.....
Episode 10 Part 1: Trauma Pearls and Pitfalls
In this episode on Trauma Pearls and Pitfalls, Dr. Dave MacKinnon and Dr. Mike Brzozowski discuss the latest in trauma controversies. In Part 1 they give us some key pearls and pitfalls on traumaairway management, the value of the C-spine collar, how to clear the C-spine, vascular access options in trauma, 'Damage Control Rescuscitation', the best resuscitation fluids to use including hypertonic saline, hemostatic drugs such as Tranexamic Acid in trauma, the vulue, or lack thereof, of Recombinant Factor 7a in trauma, and the use of Prothrombin Complex Concentrates in trauma.