cardiology emergency medicine
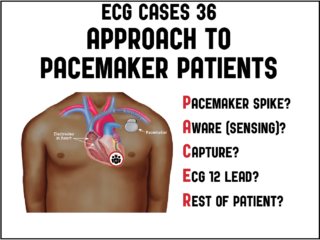
ECG Cases 36 – PACER Mnemonic for Approach to Pacemaker Patients
In this month's ECG Cases blog Dr. McLaren explains the PACER mnemonic approach to patients with pacemakers: Pacemaker spike: is it appropriately presence/absent, is there pacemaker-mediated tachycardia (apply magnet) or is there failure to pace (apply magnet to stop sensing, cardio consult)? Aware (sensing): is it normal, is there oversensing (underpacing: apply magnet) or undersensing (treat reversible causes, cardio consult). Capture: if there are pacemaker spikes is there capture, or failure to capture (treat reversible causes, cardio consult). ECG 12 lead: are there signs of hyperkalemia (extra wide QRS, peaked T) or Occlusion MI (Modified Sgarbossa Criteria) that need immediate treatment. Rest of patient: is there a complication of pacemaker insertion related to the pocket (hematoma, infection), lead (pneumothorax, DVT), or heart (pericardial perforation), or is there an emergency unrelated to the pacemaker (eg dehydration, sepsis, GI bleed)...