In this ECG Cases blog we look at seven patients with cardiac syncope, and a systematic approach to ECG interpretation…
Written by Jesse McLaren; Peer Reviewed and edited by Anton Helman. January 2020
Seven patients presented with presyncope or syncope. What’s the diagnosis?
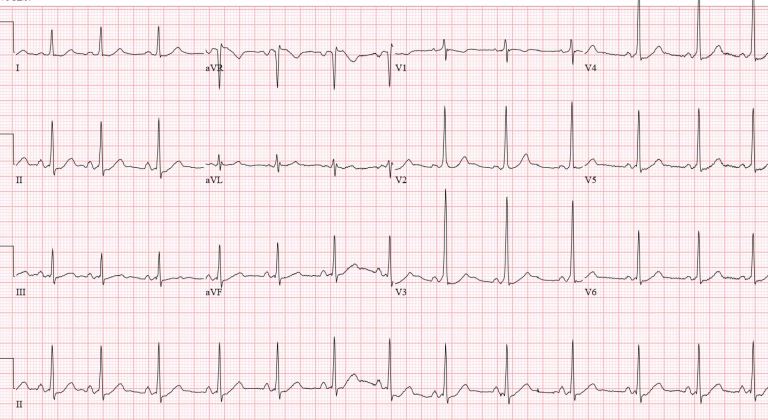
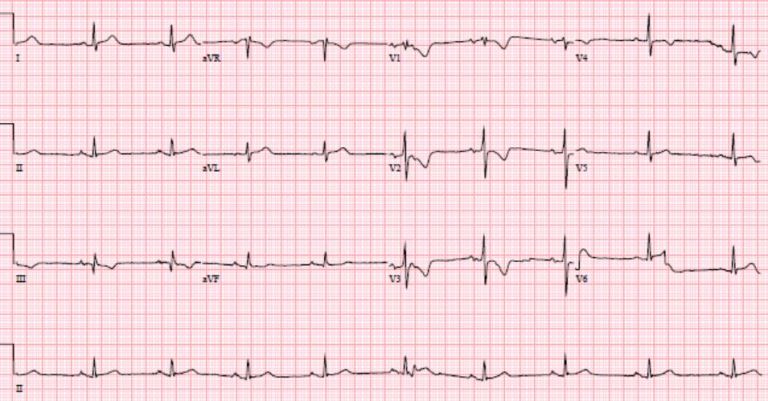
Case 1: 20yo previously well with half an hour of palpitations and presyncope, resolved
Case 2: 80yo recurring presyncope while sitting
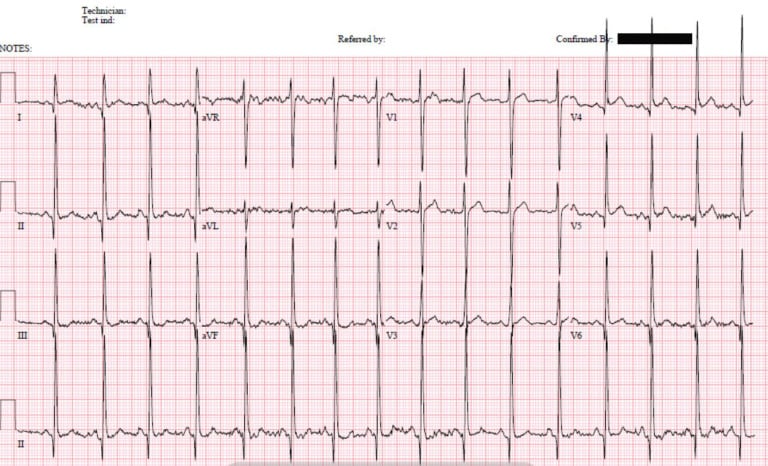
Case 3: 25yo with exertional syncope
Case 4: 70yo history of cancer, presents with shortness of breath. Shortly after ECG patient collapsed
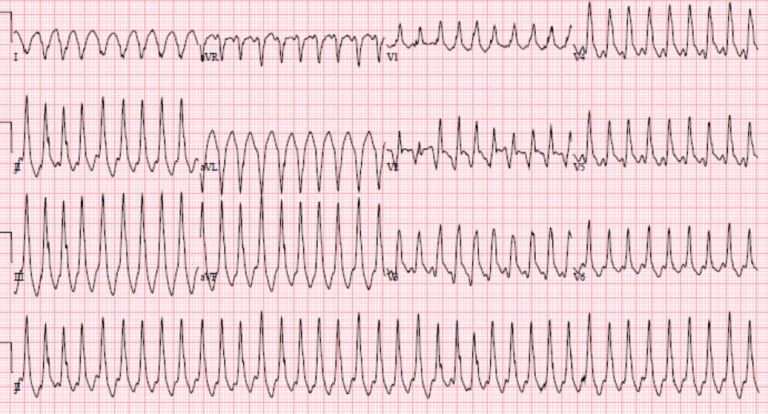
Case 5: 70yo unwell. After ECG patient collapsed
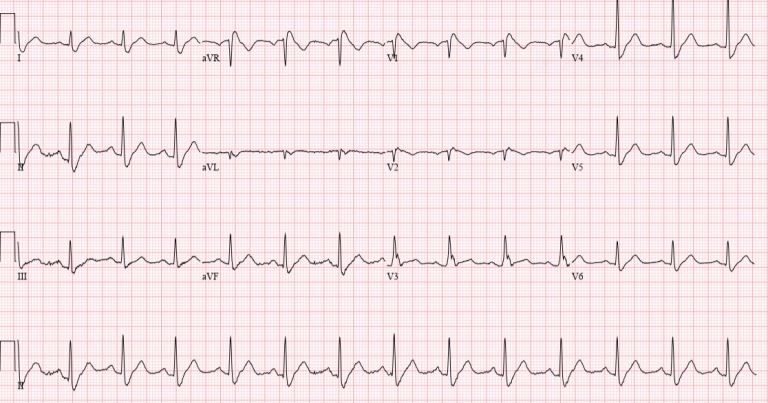
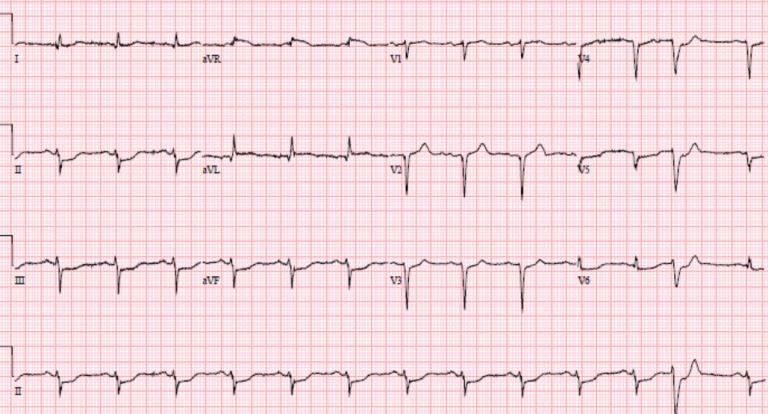
Case 6: 60yo chest pain then syncope
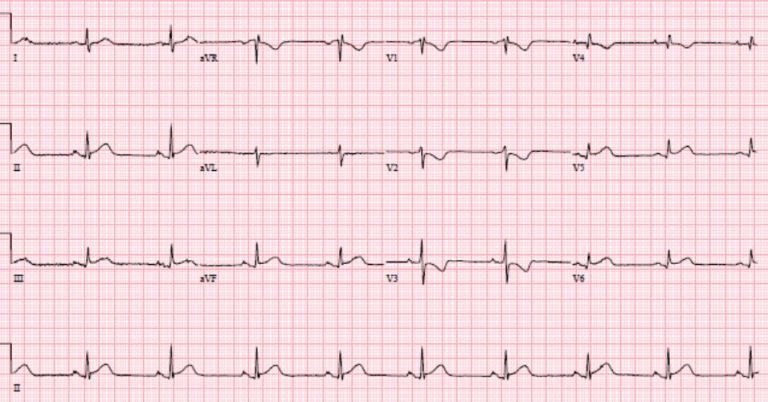
Case 7: 60yo syncope, BP 70. First ECG then post-cardioversion ECG
Cardiac syncope
The 2018 ESC guidelines for the diagnosis and management of syncope classifies syncope as reflex (vasovagal, situational or carotid sinus), orthostatic (drug-induced, volume depletion, or autonomic), or cardiac. The latter group can be caused by
- arrhythmia
- bradycardia: sinus or AV conduction disease
- tachycardia: supraventricular or ventricular
- structural
- tamponade
- ACS
- aortic stenosis
- hypertrophic cardiomyopathy (HCM)
- cardiac mass
- prosthetic valve dysfunction
- cardiopulmonary
- PE
- aortic dissection
- pulmonary hypertension
High risk features on history include: syncope with exertion or while supine, preceded by palpitations, family history of sudden death at a young age, or history of heart disease. Fore more on syncope, check out EM cases episode 25: pediatric syncope and adult syncope.
There are many different mnemonics for ECG findings in cardiac syncope, but the same systematic approach to any ECG interpretation will identify them. Just follow the HEARTS.
- Heart rate/rhythm
- tachy
- brady
- Electrical conduction
- PR long (AV block) or short+delta (WPW)
- QRS wide: BBB
- QT prolongation
- Axis
- right: PHTN, PE, LPFB
- left: LAFB
- R wave size/progression
- early R wave: RBBB, WPW type A, posterior MI, pulmonary hypertension
- late R wave: cardiomyopathy
- high voltages: hypertrophy
- low voltages: pericardial effusion
- Tension (hypertrophy)
- aortic stenosis
- HCM
- ST/T wave changes
- inherited: ARVD, Brugada
- ischemic: ACS, PE, dissection
Back to the cases
Case 1: WPW
- HR/rhythm: NSR.
- Electrical conduction: short PR with delta wave in precordial leads.
- Axis: normal.
- R wave: early progression.
- Tension: none.
- ST/ T changes: mild anterior ST depression, discordant to delta.
Diagnosis: WPW. Referred for ablatation
Case 2: “trifascicular block”
- HR/rhythm: sinus brady.
- Electrical conduction: first degree AV block + RBBB + LAFB.
- Axis: left (from LAFB).
- R wave: early (from RBBB)
- Tension: none
- ST/T wave changes: none
Diagnosis: bifascicular block with first degree AV block. Admitted for pacemaker
Case 3: HCM
- HR/rhythm: borderline sinus tach
- Electrical conduction: normal
- Axis: normal
- R wave: large voltages with deep inferolateral Q waves
- Tension: LVH
- ST/T wave: no changes
POCUS: HCM
Case 4: ECG concerning for pericardial effusion but patient had PE
- HR/rhythm: sinus tach
- Electrical conduction: normal
- Axis: normal
- R wave: small voltages
- Tension: none
- ST/T wave: no significance changes
POCUS: no pericardial effusion but RV>LV. Patient arrested, achieved ROSC after tPA and CT showed massive PE.
Case 5: Brugada
- HR/rhythm: NSR
- Electrical conduction: RBBB
- Axis: normal
- R wave: normal size/progression
- Tension: none
- ST/T wave: V1-2 coved ST elevation
Diagnosis: Brugada. Patient had VF arrest shortly after ECG, was cardioverted and admitted for ICD.
Case 6: posterior MI
- HR/rhytm: sinus bradycardia
- Electrical conduction: normal
- Axis: normal
- R wave: normal size/progression
- Tension: none
- ST/T wave: anterior ST depression with T wave inversion.
No early R waves/right axis to suggest pulmonary hypertension, no other features to suggest PE, no epsilon waves to suggest ARVD. Posterior leads showed ST elevation and cath lab activated: occluded circumflex artery
Case 7: VT then diffuse ST depression with reciprocal ST elevation in AVR
- HR/rhythm: VT cardioverted into junctional rhythm
- Electrical conduction: RBBB + LAFB
- Axis: left (from LAFB)
- R wave: RBBB superimposed on anterior Q and delayed R wave progression
- Tension: none
- ST/T wave: diffuse ST depression with reciprocal elevation in aVR. This pattern can be seen post-cardioversion, but this patient also had anterior Q waves and a bifasicular block
Repeat ECG:
- HR: NSR with PVC
- Electrical conduction: resolved RBBB, ongoing LAFB
- Axis: left (from LAFB)
- R wave: anterior Q wave and delayed R wave progression
- Tension: none
- ST/T wave: ongoing diffuse ST depression with reciprocal ST elevation in aVR.
Dynamic RBBB/LAFB + ST elevation is associated with left main or LAD occlusion. Cath lab activated: LAD occlusion
Take home points on ECG interpretation for cardiac syncope
- Cardiac syncope often has high-risk features on history: palpitations or no prodrome (arrhythmogenic), exertional (HCM, aortic stenosis), or chest pain (ACS, PE, dissection)
- Systematic ECG interpretation can identify abnormalities in Heart rate/rhythm, Electrical conduction, Axis, R wave, Tension, and ST/T wave changes
- POCUS is a helpful adjunct
References for ECG Cases 5: cardiac syncope
- Brignole M, Moya A, de Lange F, et al. 2018 ESC guidelines for the diagnosis and management of syncope. Eur Herat J 2018 June 1;39(21):1883-1948
- Dovgalyuk J, Holstege C, Mattu A and Brady W. The electrocardiogram in the patient with syncope. Am J Emerg Med 2007;25:688-701







Great post Jesse!
When the cause is not obvious, I also found useful the 2nd ECG look to explore WOBBLER via Cliff Reid https://resus.me/wobbler/
WPW
Obstructed AV pathway
Bi-trifascicular block
Brugada
LVH
Epsilon wave (arrhythmogenic RV cardiomyopathy)
Repolarization abnormalities (long/short QT)
Thanks for sharing your knowledge
roberto
Thanks!
2nd ECG case cant be AVB1 – ( First degree ) PQ Hence RBBB + LAH = Bifacikular block
PQ < 220 ms
AVB1 is PR> 200 (http://www.onlinejacc.org/content/accj/early/2018/11/08/j.jacc.2018.10.044.full.pdf), which is borderline in this case.
great effort.thank you sir