In this ECG Cases blog we look at 8 patients with potentially ischemic symptoms, none of whom had STEMI on the 12 lead ECG. Which had occlusion MI?
Written by Jesse McLaren; Peer Reviewed and edited by Anton Helman. February 2020
Eight patients presented with potentially ischemic symptoms. Which had an acute coronary occlusion?
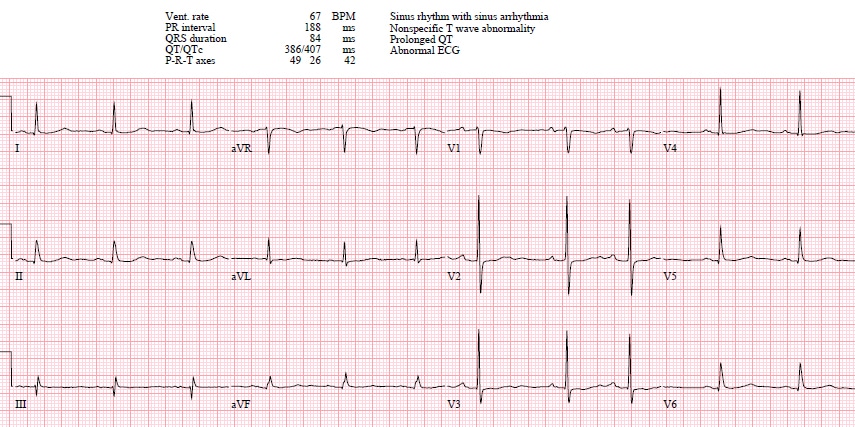
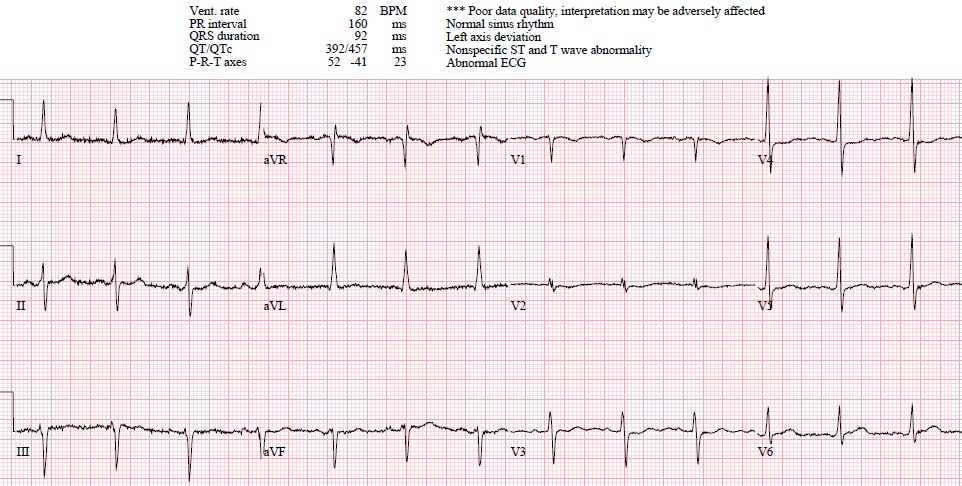
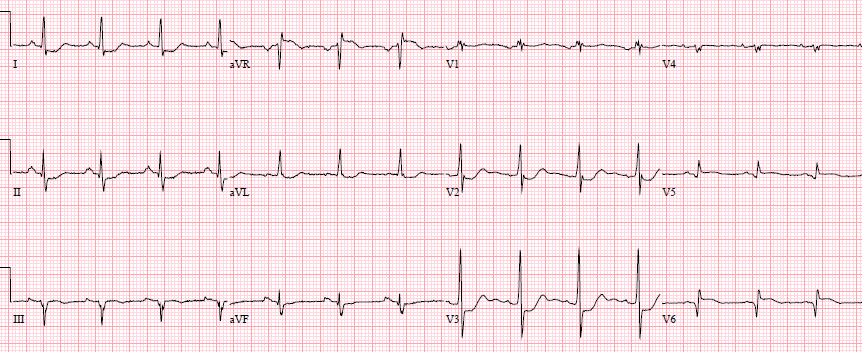
Case 1: 80yo with one day weak/dizzy, no prior ECG
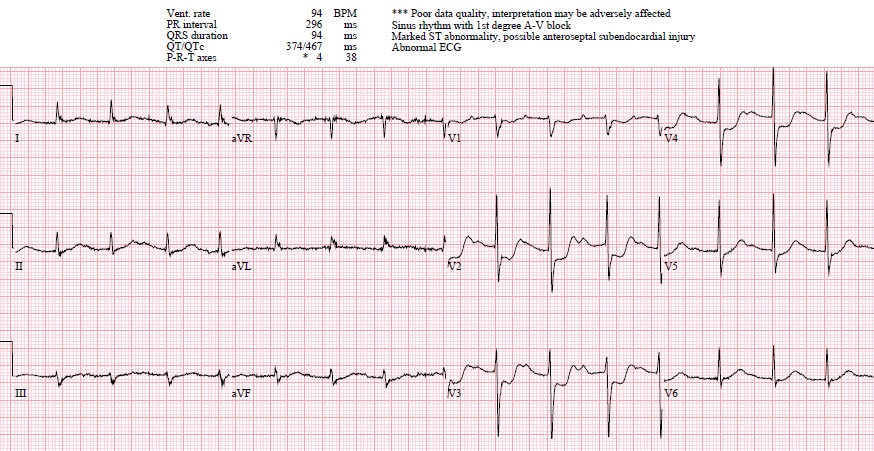
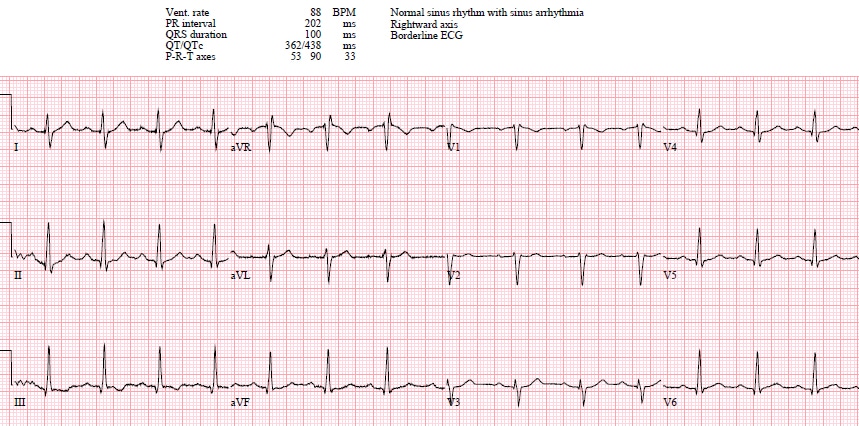
Cases 2: Same patient years later, with acute chest pain
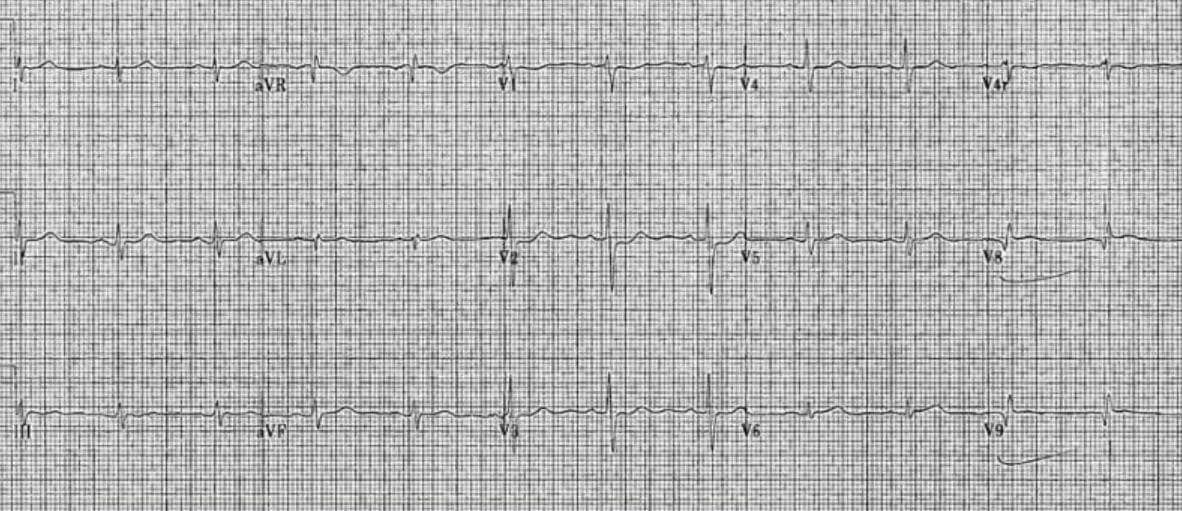
Case 3: 40yo acute chest pain with diaphoresis, no prior ECG
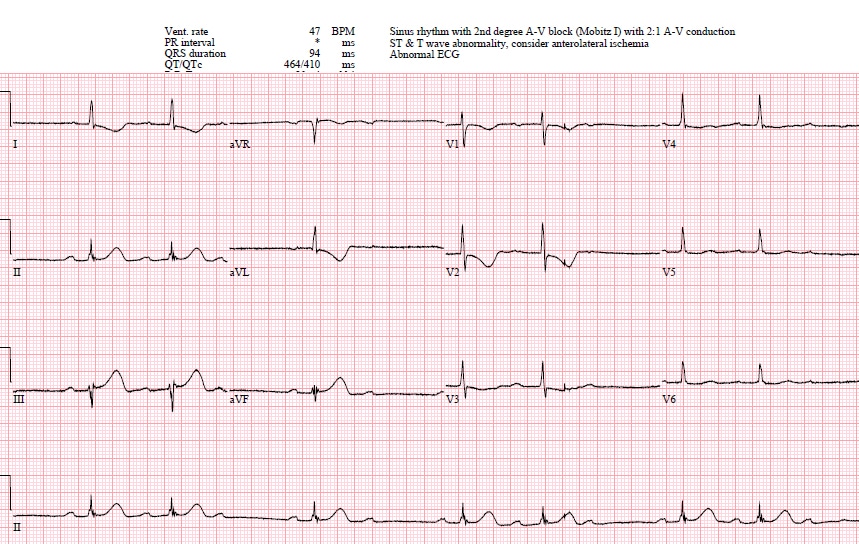
Case 4: 75yo acute chest pain, no prior ECG
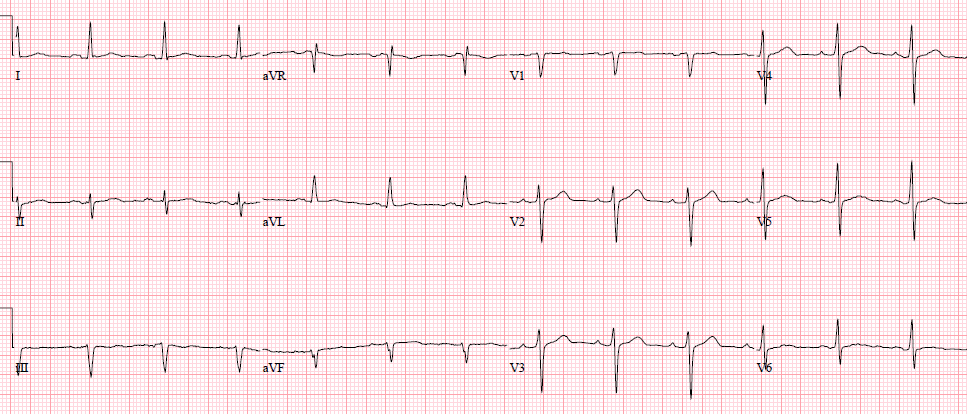
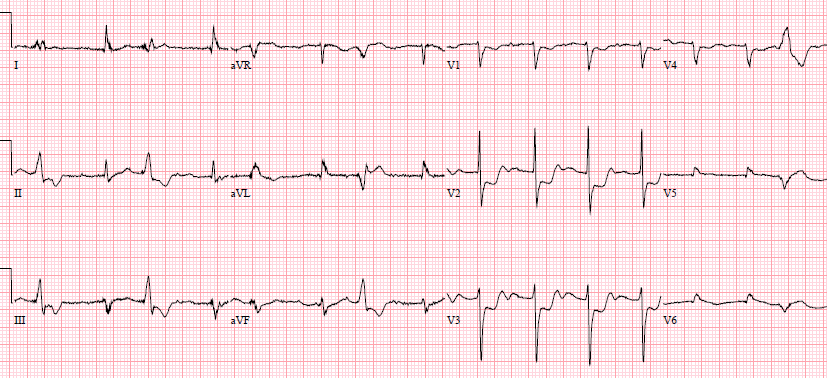
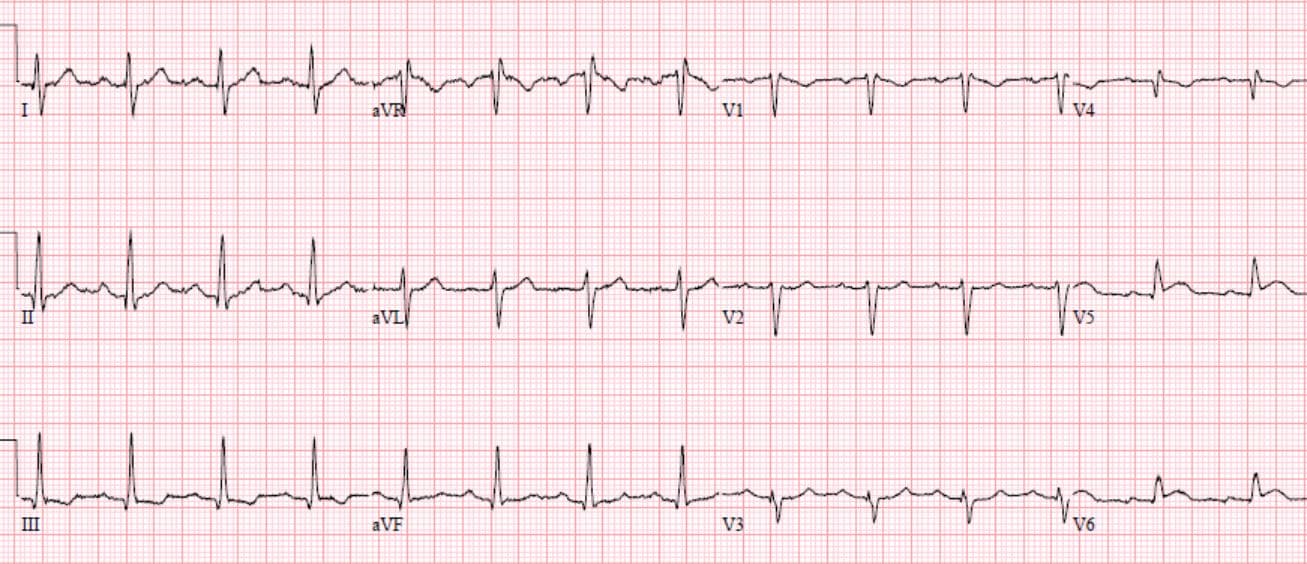
Case 5: 60yo with acute chest pain, old then new ECG
Case 6: 55yo with recurring bilateral shoulder pain, now constant; no prior ECG
Case 7: 65yo acute chest pain, no prior ECG
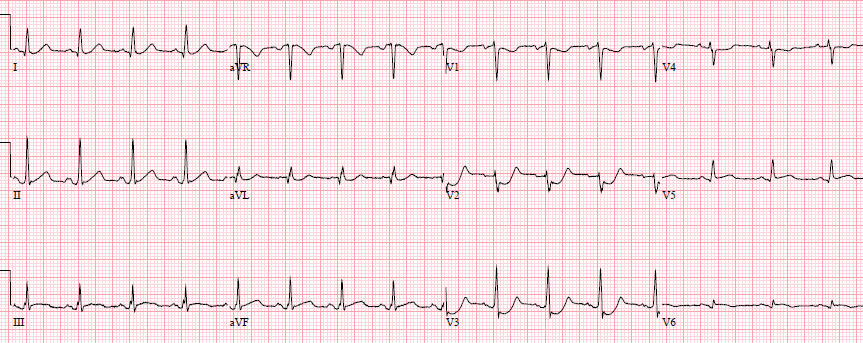
Case 8: 60yo exertional chest pain now constant; old then new ECG
Posterior MI
Posterior myocardial infarctions have always had a tendency of being overlooked, not because they are invisible on the 12 lead ECG but because they do not conform to the dominant paradigm. When MIs were dichotomized as Q wave vs non-Q wave MI, posterior MIs were missed because they did not produce Q waves. A study in 1964 found that posterior MIs produce tall anterior R waves, and differentiated it from other causes (pediatric ECG, WPW, RBBB, RVH, and normal variant). But “because of this absence of pathologic Q waves, strictly posterior infarction is one of the most commonly overlooked electrocardiographic abnormalities.” (1).
When the paradigm changed to STEMI vs NSTEMI, posterior MIs were still missed because they didn’t produce ST elevation on the 12 lead. A study in 1987 found that the ST depression in posterior MI is isolated to the right precordial leads, is horizontal in morphology, and is associated with upright T waves–all features that helped to differentiate it from subendocardial ischemia and other causes of ST depression. But “the arbitrary exclusion of all patients with prolonged chest pain and precordial ST segment depression appears to categorically eliminate patients with evolving posterior MI, whose infarct related coronary artery would be, in most instances, either the left circumflex coronary or dominant right coronary artery with sizable posterior descending or posterolateral branches.” (2)
Decades later, posterior MI is still under-recognized: among nearly 1200 ACS patients with ST depression isolated to leads V1-4, a quarter had occluded arteries (half of which were circumflex), but the average time from ECG to reperfusion was 29 hours, leading to a higher mortality rate. (3) A paradigm shift from STEMI to Occlusion MI (OMI) puts the focus back on the diagnostic signs of occlusion that don’t require Q waves or ST elevation thresholds. As a review of posterior MI summarized,
“From the perspective of the standard 12-lead EKG, the ‘typical’ electrocardiographic findings indicative of acute transmural myocardial infarction will be reversed. This reversal results from the fact that the endocardial surface of the posterior wall faces the anterior precordial leads (V1-3) in the standard 12-led EKG. In other words, STD, prominent R waves, and upright T waves in leads V1 through V3–‘when reversed’–represent STE, Q waves, and T wave inversion, respectively, of acute PMI. If one considers the ‘reversed nature’ of these electrocardiographic abnormalities when applied to the posterior wall, the findings assume a more recognizable, ominous meaning…The presence of an upright T wave, although more commonly seen in patients with posterior wall infarction, is not a reliable indicator of PMI. The polarity of the right precordial T wave may, in fact, be related to the age of the infarction with early PMI presenting with inverted T waves and more established infarcts manifesting with upright T waves.”(4)
Posterior leads have drawn attention to posterior MI because they can reveal ST elevation—thereby earning inclusion as a “STEMI.” But posterior leads have their own limitations. A 1999 study of circumflex occlusion found only a third met inferior or lateral STEMI criteria on the 12 lead but half had 1mm ST elevation on posterior leads, including a quarter where ST elevation was only present on the posterior leads—showing the value of posterior leads. But 12% had anterior ST depression without significant posterior ST elevation, showing the limits of posterior leads.(5) A 2001 study found that only 53% of posterior MIs from circumflex occlusions had ST elevation of 1mm in posterior leads, which increased to 94% if the ST elevation threshold was reduced to 0.5mm—leaving 6% that had no posterior ST elevation(5). This has been incorporated into the Fourth Universal Definition of MI, which states that “isolated ST-segment depression 0.5mm in leads V1-3 may indicate left circumflex occlusion and can best be captured using posterior leads…a cut-off point of 0.5 ST elevation is recommended in leads V7-9; specificity is increased at a cut-off point of 1mm ST elevation and this cut-off point should be used in men <40 years old.(7)
Back to the cases
Case 1: Baseline ECG
- HR/rhythm: NSR
- Electrical conduction: normal intervals, no blocks
- Axis: normal
- R-wave: tall R wave in V2
- Tension: no hypertrophy
- ST/T wave changes: anterior horizontal ST segments with any ST elevation (pseudonormal)
Impression: Possible posterior MI, but could be old or baseline, in patient without classic symptoms; posterior leads done:
No ST elevation. Serial ECGs unchanged and serial trops negative.
Cases 2: Obvious posterior MI, cath lab activated despite equivocal posterior leads
- HR/rhythm: borderline sinus tach
- Electrical conduction: first degree heart block
- Axis: normal
- R wave: tall R wave in V2
- Tension: none
- ST/T: horizontal/downsloping ST depression V1-4 and upright T waves
Impression: Classic ECG for Posterior MI; posterior leads done:
Minimal elevation in V9 so cardiology consulted stat. Cath lab activation: 90% circumflex occlusion, peak trop 50,000. Discharge diagnosis: “NSTEMI”
Case 3: Obvious posterior MI, delayed reperfusion due to posterior leads
- HR/rhythm: borderline sinus tach
- Electrical conduction: normal
- Axis: normal
- R wave: tall R wave in V2
- Tension: none
- ST/T: dowsloping ST depression V1-4 and upright T waves
Impression: Classic ECG for posterior MI; posterior leads done:
Minimal ST elevation. Stat cardiology consult: “no STEMI”. Pain refractory to asa, plaxix, nitro, heparin, and cardiology consulted an hour later. Admitted as NSTEMI and cath 18 hours later: 95% circumflex occlusion.
Case 4: Obvious inferoposterior MI, no posterior leads done
- HR/rhythm: sinus bradycardia
- Electrical conduction: Wenckeback block
- Axis: normal
- R wave: tall R wave in V2
- Tension: none
- ST/T: hyperacute inferior T waves with reciprocal change in aVL and I, and downsloping ST depression V2-3 with T wave inversion in V2
Impression: No STEMI criteria but diagnostic of infero-posterior occlusion MI (OMI), likely from RCA occlusion affecting the AV node. Taken by paramedics directly to cath lab: dominant RCA occlusion, complicated by heart block requiring temporary pacing. First trop negative, peak 20,000.
Case 5: Subtle posterior MI, delayed diagnosis
- HR/rhythm: NSR
- Electrical conduction: LAFB
- Axis: left
- R wave: normal
- Tension: none
- ST/T: compared to old there is mild horizontal ST depression V2-4 and T wave flattening
Possible posterior MI was not recognized. Given asa and nitro. First trop negative but pain persisted. Posterior leads done:
Clear ST elevation V8-9. Cath lab activated: circumflex occlusion.
Case 6: Subtle posterior MI, delayed diagnosis
- HR/rhythm: NSR
- Electrical conduction: normal
- Axis: normal
- R wave: tall in V2
- ST/T: pseudonormal ST segment in V2 and upsloping ST depression V3-5
Impression: ST depression not confined to anterior leads, and tall R wave in V2, possible posterior MI; when trop came back 7,000 posterior leads were done:
Now deeper ST depression in V2-3 and ST elevation V9, cath lab activated: circumflex occlusion. Peak trop 50,000.
Case 7: Subtle posterior MI, rapid diagnosis
- HR/rhythm: NSR
- Electrical conduction: normal
- Axis: normal
- R wave: normal
- Tension: none
- ST/T: horizontal anterior ST depression V2-3
Impression: Another ischemic ECG labelled “normal” by the computer. ST depression isolated to V2-3 concerning for posterior MI. Posterior leads done:
Mild ST elevation V8-9, cath lab activated: circumflex occlusion. First trop 150, peak trop 40,000
Case 8: Subtle posterior MI, rapid diagnosis
- HR/rhythm; NSR
- Electrical conduction: normal
- Axis: normal
- R wave: normal
- Tension: none
- ST/T: compared with the old ECG there is relative ST depression (pseudonormalization) in V2-3; (also old and incidental S1Q3T3, neither sensitive nor specific for PE)
Impression: Relative ST depression in V2-3, possible posterior MI; posterior leads done:
ST elevation V8-9. Cath lab activated: occlusion of OM branch of circumflex. First trop negative, peak 50,000.
Take home points on posterior MI
- Posterior MI won’t produce ST elevation or Q waves on the 12 lead, but it can be recognized by
- Tall anterior R waves (especially new, and not secondary to RBBB/WPW/RVH)
- ST depression (including pseudonormalization) isolated to the anterior leads, especially horizontal, and often associated with upright T waves
- Associated inferior or lateral hyperacute T waves or subtle elevation
- Posterior leads are helpful for subtle cases, but if the occlusion is obvious on the 12 lead the posterior leads can be falsely reassuring
- If in doubt: serial ECG, stat cardiology consult
References for ECG Cases 6: Posterior MI
1. Perloff JK. The recognition of strictly posterior myocardial infarction by conventional scalar electrocardiography. Circulation. 1964;30:706-18.
2. Boden WE, Kleiger RE, Gibson RS, et al. Electrocardiographic evolution of posterior acute myocardial infarction: importance of early precordial ST-segment depression. Am J Cardiol. 1987;59(8):782-7.
3. Pride YB, Tung P, Mohanavelu S, et al. Angiographic and clinical outcomes among patients with acute coronary syndromes presenting with isolated anterior ST-segment depression: a TRITON-TIMI 38 (Trial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet Inhibition With Prasugrel-Thrombolysis in Myocardial Infarction 38) substudy. JACC Cardiovasc Interv 2010 Aug;3(8):806-11
4. Brady WJ, Erling B, Pollack M, Chan TC. Electrocardiographic manifestations: acute posterior wall myocardial infarction. J Emerg Med. 2001;20(4):391-401.
5. Khaw K, Moreyra AE, Tannenbaum AK, Hosler MN, Brewer TJ, Agarwal JB. Improved detection of posterior myocardial wall ischemia with the 15-lead electrocardiogram. Am Heart J. 1999;138(5 Pt 1):934-40.
6. Wung SF, Drew BJ. New electrocardiographic criteria for posterior wall acute myocardial ischemia validated by a percutaneous transluminal coronary angioplasty model of acute myocardial infarction. Am J Cardiol. 2001 Apr 15;87(8):970-4; A4.
7. Thygesen K, Alpert JS, Jaffe AS et al. Fourth universal definition of myocardial infarction (2018). Eur Heart J 2019 Jan 14;40(3):237-269











Thank you for this excellent summary.
thanks!
Detailed explanation with excellent examples. Without your analysis, for sure many of us will not able to realize these are posterior MI. Thanks for your teaching.