In this ECG Cases blog we look at 10 patients who presented with acute symptoms, whose ECGs revealed the “STEMI-equivalent” pattern of ST elevation in aVR with diffuse ST depression. Which had acute coronary occlusion?
Written by Jesse McLaren; Peer Reviewed and edited by Anton Helman. March 2020
10 patients presented with acute symptoms and ECGs that had the “STEMI-equivalent” pattern of ST elevation in aVR and diffuse ST depression. Which had acute coronary occlusion?
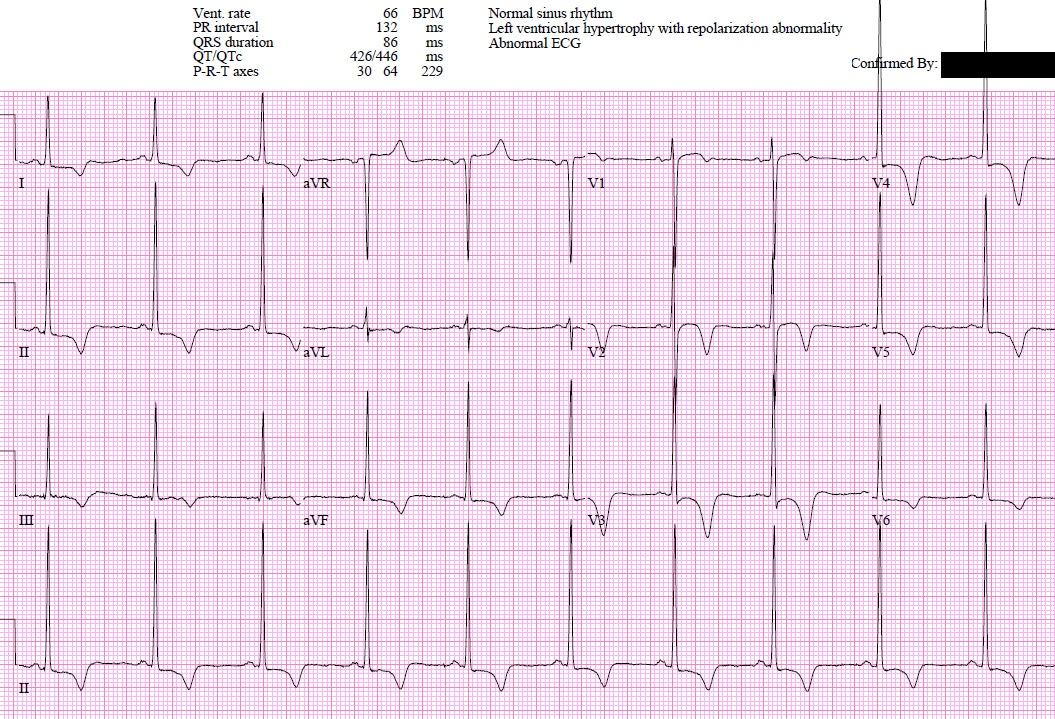
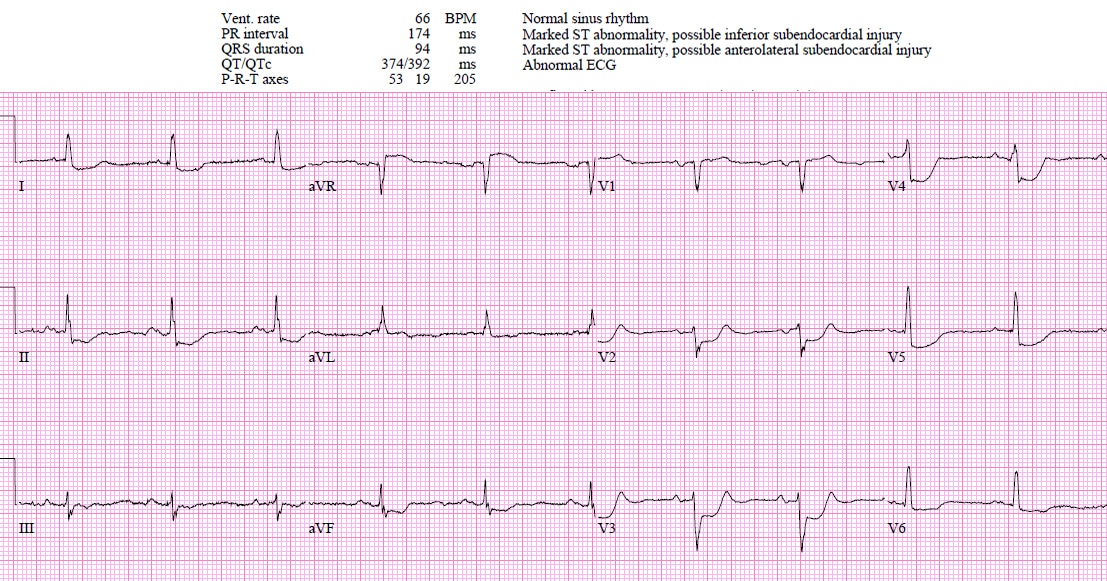
Patient 1: 70yo with two hours of chest pain. Normal vitals.
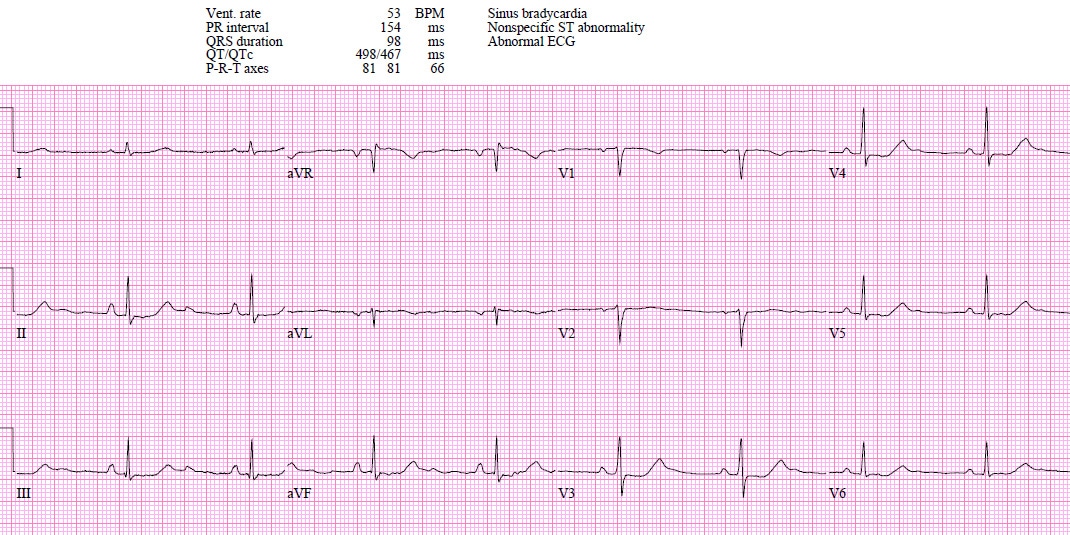
Patient 2: 35yo with a day of vomiting and weakness. Normal vitals.
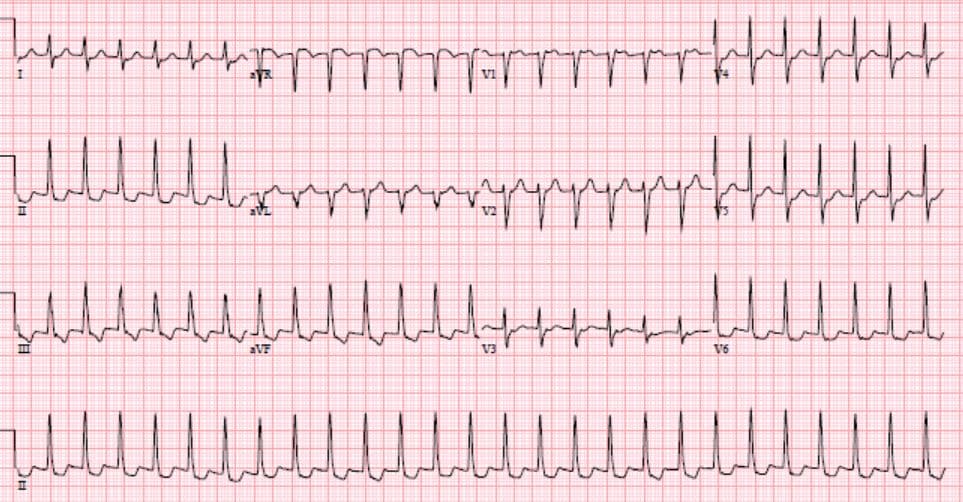
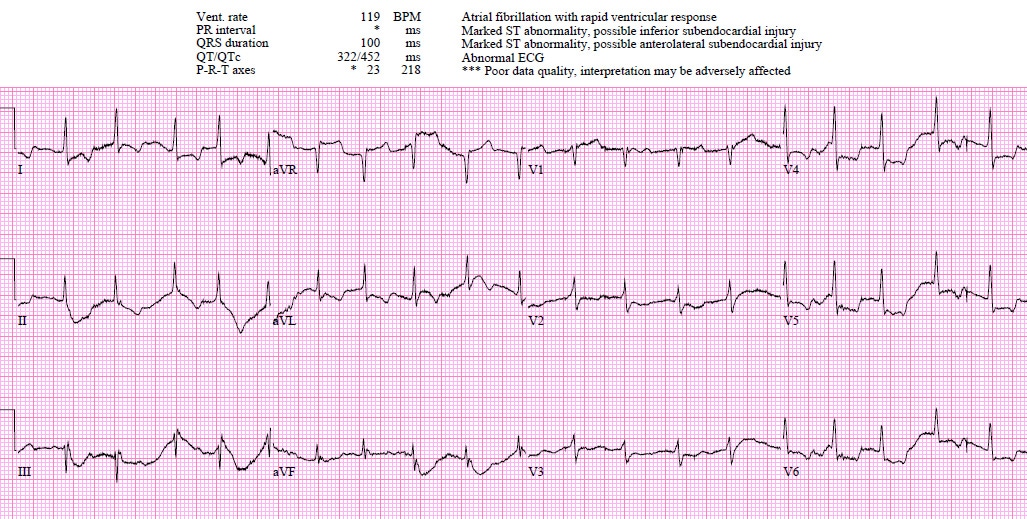
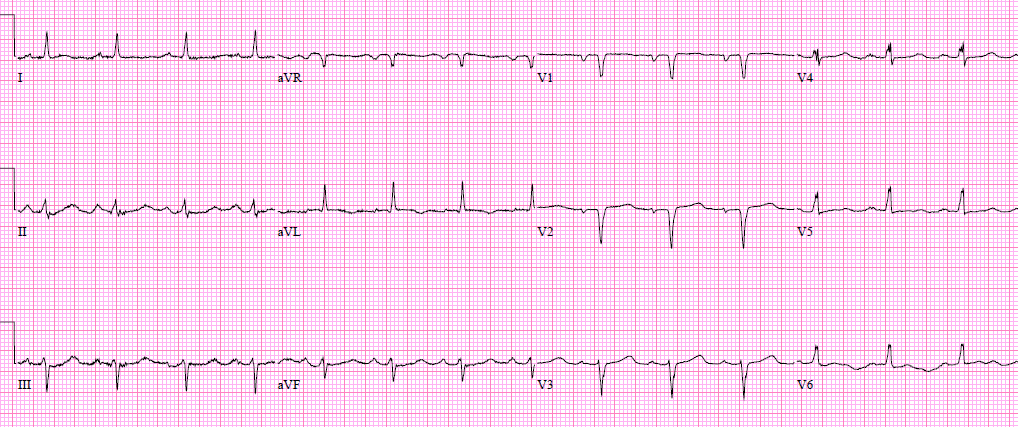
Patient 3: 60yo sudden palpitations and chest pressure. Tachycardic, normal BP and other vitals.
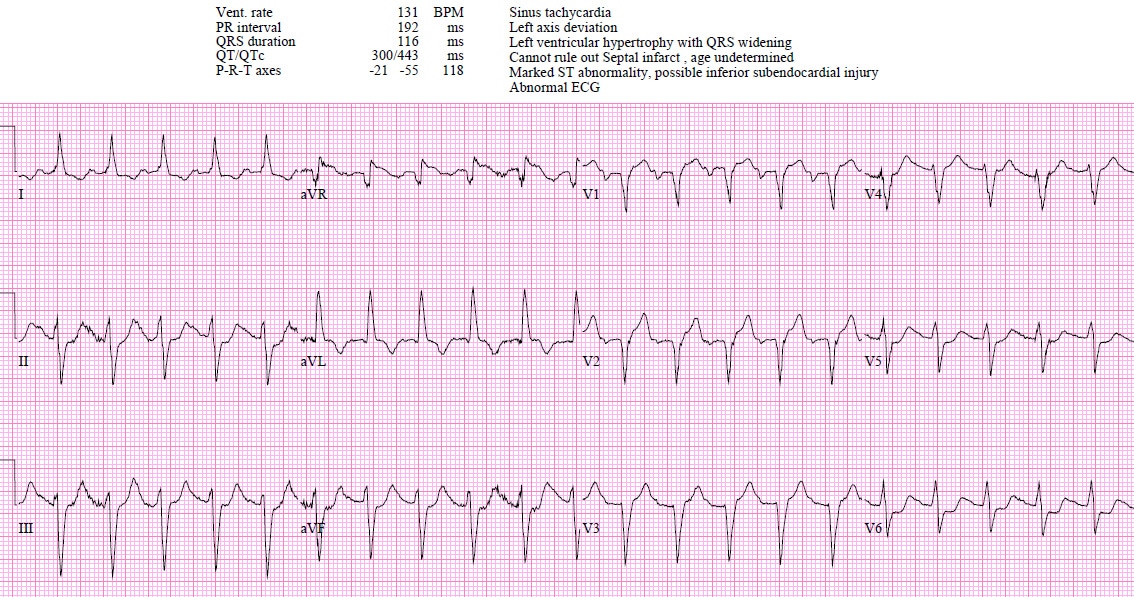
Patient 4: 90yo with few days progressive lethargy and shortness of breath. HR 120, BP 80s, O2 80s, temp 35.0.
Patient 5: 50yo with chest pressure, shortness of breath, nausea, lightheaded. HR 110, BP 90s, sat 90s, lungs clear.
Patient 6: 75yo with a few hours of chest pain and shortness of breath. HR 130, BP 110, sat 85%. Bilateral crackles on auscultation and poor LV on POCUS.
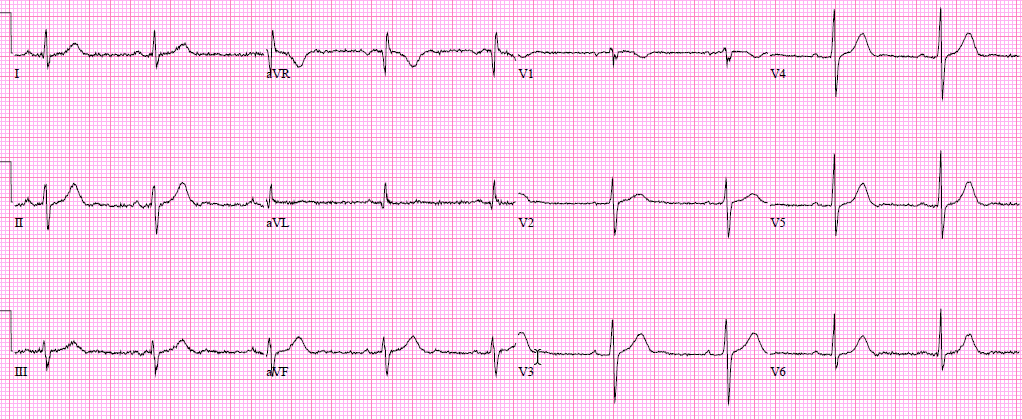
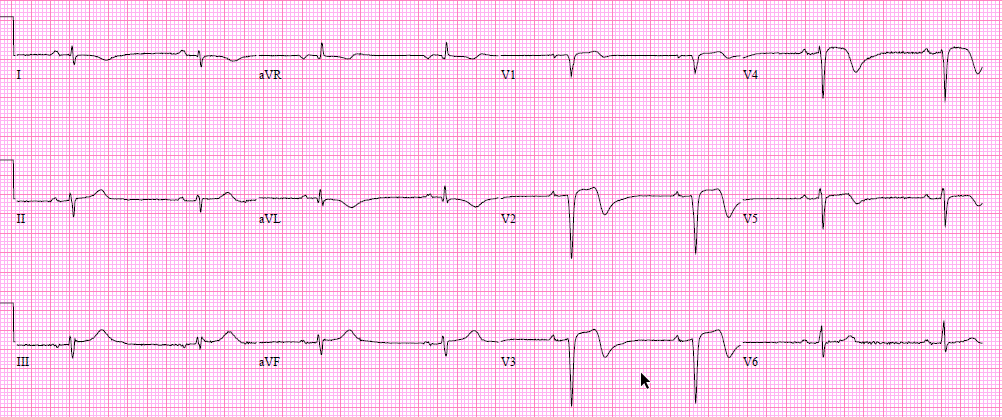
Patient 7: 70yo with 5 hours of chest pain. Old then new ECG:
Patient 8: 50yo exertional chest pain to bilateral arms now constant for two hours. Normal vitals.
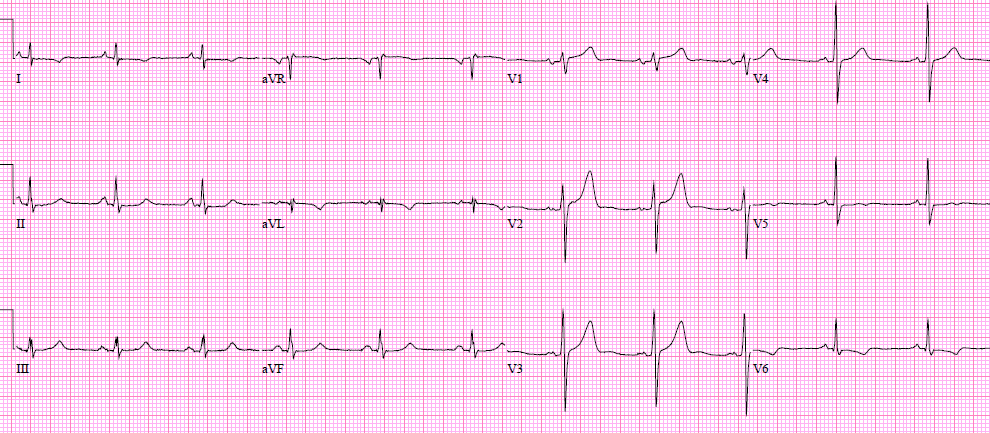
Patient 9: 70yo CABG with exertional chest pain now unresponsive to nitro. Normal vitals. Old then new ECG:
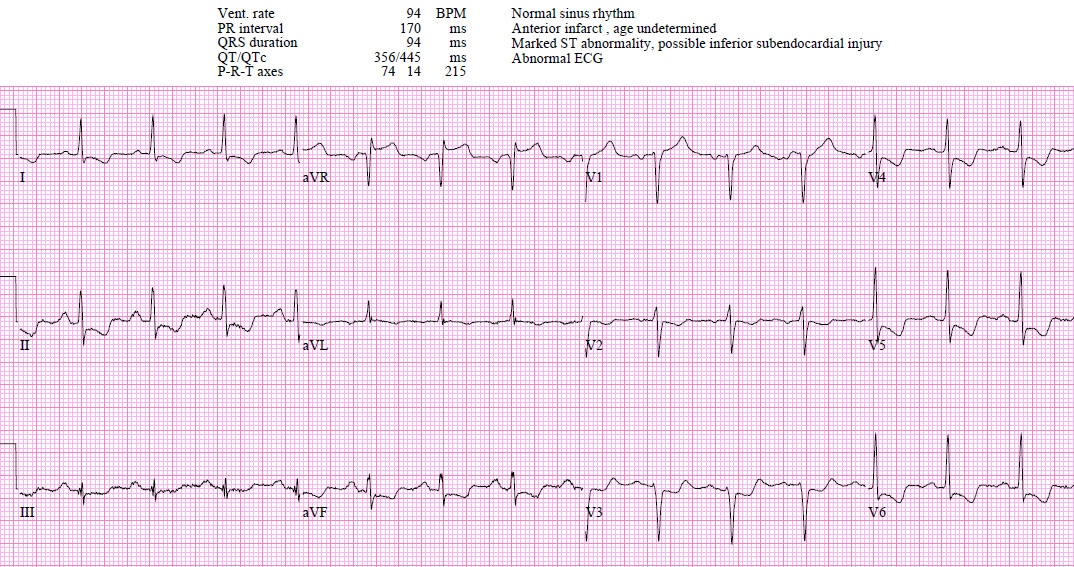
Patient 10: 80yo with two days of chest pain. Normal vitals.
Diffuse ST depression with reciprocal ST elevation in aVR
aVR has gone from the “forgotten lead” to be equated with the worst coronary occlusion: the 2013 AHA/ACC STEMI guideline notes that “multilead ST depression with coexistent ST elevation in lead aVR has been described in patients with left main or proximal left anterior descending artery occlusion”[1] and the 2018 Fourth Universal Definition of MI added the update, “ST-segment elevation in lead aVR with specific repolarization patterns, as a STEMI equivalent.”[2] But the latter describe two situations of ST elevation in aVR: STE-aVR as a “STEMI-equivalent” (“ST-segment depression >1mm in six leads, which may be associated with ST-segment elevation in leads aVR or lead V1 and haemodynamic compromise, is suggestive evidence of multivessel disease or left main disease”), and STE-aVR as part of STEMI (“ST-elevation in lead aVR>1mm may accompany anterior or inferior STEMI, and is associated with increased 30 day mortality in patients with acute MI.”)
Because STEMI criteria and STEMI-equivalents focus on ST elevation, the focus for this pattern has been on the ST elevation in aVR, rather than on the ST depression in all the the other leads. But it’s not just ACS that can cause diffuse ST depression with ST elevation in aVR. A recent analysis of this pattern in 99 patients found that a third were tachy-dysrhythmias, a third were non-cardiac shock states (septic shock, hemorrhagic shock, dissection, PE), and a third were ACS. Only 10% had a culprit lesion, leading the authors to conclude that “routine STEMI activation in STE-aVR for emergent revascularization is not warranted.” This study included all patients with this ECG pattern irrespective of presentation (including septic shock) or ECG confounders (including LBBB/LVH that cause secondary ST depression, and tachy-arrhythmias that cause transient ST depression). Despite this broad inclusion, the overall population was very high risk: a third presented in cardiac arrest, and the in-hospital mortality rate was also a third (compared to 6% for STEMI without STE-aVR). In a more selective study of those patients undergoing angiography for diffuse ST depression with reciprocal STE in aVR (excluding LBBB and LVH), half required revascularization, of which half required CABG.[4]
As a review summarized, “although nearly half of patients with >1mm STE in aVR due to ACS will require coronary artery bypass surgery for revascularization, the infarct artery is often not the LM, but rather the LAD or severe 3-vessel disease. More importantly, such ECG findings are frequently due to nonocclusive etiologies (eg, baseline LVH, demand ischemia secondary to respiratory failure, aortic stenosis, hemorrhagic shock)…thus, a number of expert reviews emphasize the low specificity of the aVR STE pattern, preferring to label it as circumferential subendocardial ischemia; in this syndrome, STE in aVR is reciprocal STE, reciprocal to an STD vector toward leads II and V5…some patients whose ECGs already meet conventional STEMI criteria might also have STE in lead aVR. This finding does not alter the need to pursue emergent reperfusion, although it might suggest a poorer prognosis.”[5]
So it’s more helpful to think of STE-aVR as reciprocal to diffuse ST depression, rather than the other way around. Then the question becomes, what is causing diffuse ST depression? Is it simply a repolarization abnormality (LVH, LBBB) or rate-related (eg SVT), is it from a metabolic/toxic cause (hypokalemia, dig toxicity), is it from a non-ACS shock state (sepsis, hemorrhage, dissection, PE), or is it from acute coronary occlusion (in addition to other signs of occlusion, or as the only sign).
Back to the cases
Patient 1: Hypertrophic Cardiomyopathy (HCM), unnecessary cath lab activation.
- HR/rhythm: normal
- Electrical conduction: normal intervals
- Axis: normal
- R wave: large voltages, normal transition
- Tension: LVH
- ST/T wave: diffuse ST depression (with reciprocal ST elevation in aVR) and T wave inversion
ST/T wave changes are secondary repolarization abnormalities from significant LVH. Serial ECG unchanged, normal coronaries on angio, and hypertrophic cardiomyopathy on echo.
Patient 2: hypokalemia, diagnosed after labs.
- HR/rhythm: sinus brady
- Electrical: normal PR/QRS/QT, U waves seen most clearly in inferior leads
- Axis: normal
- R-wave: normal height/transition
- Tension: no hypertrophy
- ST/T: diffuse ST depression (and reciprocal ST elevation in aVR)
Weakness from vomiting associated with diffuse ST depression and and U waves is classic for hypokalemia. Potassium level 2.2. After potassium replacement, all changes resolved:
Patient 3: SVT, cardioverted.
- HR/rhythm: SVT
- Electrical: normal QRS
- Axis: normal
- R wave: normal height/transition
- Tension: no hypertrophy
- ST/T: diffuse ST depression and reciprocal ST elevation in aVR
ST/T wave changes secondary to rapid heart rate. Resolved after cardioversion:
Patient 4: septic shock, treated.
- HR/rhythm: rapid AF
- Electrical: normal QRS/QT
- Axis: normal
- R wave: normal size, early transition
- Tension: no hypertrophy
- ST/T: diffuse ST depression and reciprocal ST elevation in aVR, lateral T wave inversion
Diffuse ST depression from shock and compensatory tachycardia. Stat cardiology consult: normal LV on echo. Diagnosed as septic shock and treated with fluids, antibiotics, pressors.
Patient 5: massive GI bleed initially treated as ACS.
- HR/rhythm: sinus tach
- Electrical: normal intervals
- Axis: normal
- R-wave: normal
- Tension: no hypertrophy
- ST/T: diffuse ST depression and reciprocal ST elevation in aVR
Code STEMI activated, treated with aspirin, plavix, heparin. Then hemoglobin came back at 30. Massive transfusion protocol activated, and anti-coagulants and anti-platelets reversed. Urgent scope: bleeding ulcer.
Patient 6: LAD occlusion and acute heart failure, early diagnosis.
- HR/rhythm: sinus tach
- Electrical: normal intervals
- Axis: left axis from LAFB
- R-wave: poor R wave progression, anterior Q waves
- T: LVH criteria in aVL, but this can be seen with LAFB
- ST/T: 1-2mm ST elevation V1-3 with inferolateral ST depression and reciprocal ST elevation in aVR.
Patient in CHF on clinical exam, cath lab activated: LAD occlusion. On discharge, LAFB and ST/T wave changes resolved:
Patient 7: LAD occlusion, false cath lab cancellation.
- HR/rhythm: sinus brady
- Electrical: normal
- Axis: left from LAFB (old)
- R wave: new loss of precordial R waves and new Q wave V2-3
- Tension: no hypertrophy
- ST/T: convex ST elevation V1, hyperdynamic T waves V1-4, ST depression in multiple leads, along with reciprocal ST elevation in aVR
Multiple diagnostic signs of LAD occlusion, but didn’t meet STEMI criteria so code cancelled. Code activated when first trop positive at 150, ECG unchanged. Cath lab: proximal LAD occlusion, peak trop 50,000, EF 40% with aneurysmal apex. Discharge ECG: reperfusion T wave inversion
Patient 8: circumflex occlusion, delayed cath lab activation.
- HR/rhythm: NSR
- Electrical: normal intervals
- Axis: normal
- R-wave: normal height, delayed transition
- Tension: no hypertrophy
- ST/T: diffuse ST depression with reciprocal ST elevation in aVR
When trop came back at 800, the cath lab was activated: circumflex occlusion. Discharge ECG: reperfusion T wave inversion laterally and posteriorly (manifested as hyperacute T wave anteriorly):
Patient 9: RCA graft occlusion, early diagnosis.
- HR/rhythm: NSR
- Electrical: normal intervals
- Axis: normal
- R wave: normal
- Tension: no hypertrophy
- ST/T: old anterolateral T wave inversion, new diffuse ST depression with reciprocal ST elevation
Cath lab activated: occluded RCA graft.
Patient 10: triple vessel disease, early diagnosis.
- H/rhythm: NSR
- Electrical: normal intervals
- Axis: normal
- R wave: normal
- Tension: no hypertrophy
- ST/T: diffuse ST depression with reciprocal ST elevation in AVR
Cath lab activated: triple vessel disease treated with CABG.
Take home points on ST elevation in aVR, STEMI-equivalent?
- Diffuse ST depression, with reciprocal ST elevation in aVR, can be a baseline secondary repolarization abnormality (eg from LVH, LBBB), rate-related (eg tachydysrhythmia) or caused by a metabolic/toxic causes (eg hypokalemia, digoxin)
- Diffuse ST depression, with reciprocal ST elevation in aVR, can be represent circumferential subendocardial ischemia from any shock state (eg sepsis, GI bleed, PE, dissection), and is a high-risk finding
- If caused by ACS, this can be from any acute coronary occlusion, or multi-vessel disease, and can accompany other signs of acute coronary occlusion or be the only sign
- Clinical assessment and POCUS can help differentiate the causes, and if in doubt: stat cardiology consult
References for ECG cases 7: ST elevation in aVR, STEMI-equivalent?
- O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction. Circulation 2013, 61(4): 378-140
- Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). Eur Heart J 2019, 40: 237-269
- Harhash AA, Huang JJ, Reddy S, et al. aVR ST segment elevation: acute STEMI or not? Incidence of an acute coronary occlusion. Am J Med 2019, 132(5):622-630
- Knotts RJ, WIlson JM, Kim E, et al. Diffuse ST depression with ST elevation in aVR: is this pattern specific for global ischemia due to the left main coronary artery disease? J Electrocardiol 2013, 46(3):240-8
- Miranda DF, Lobo AS, Walsh B, et al. New insights into the use of the 12-lead electrocardiogram for diagnosing acute myocardial infarction in the emergency department. Can J of Cardiol 2018, 34: 132-145










Very informative cases and evaluation and duscussion
For medical professionals wether resistance or consultants
Thanks for the information