In this ECG Cases blog we look at 7 patients with RBBB and potentially ischemic symptoms. Which had RBBB and occlusion MI?
Written by Jesse McLaren; Peer Reviewed and edited by Anton Helman. August 2020
Seven patients presented with potentially ischemic symptoms. Which had occlusion MI?
Case 1: 70yo with chest pain. HR 140, BP 150, RR20, sat 98%. Old then new ECG:
Case 2: 70yo with syncope. AVSS. Old then new ECG:
Case 3: 75yo with an hour of chest pain. HR 90, BP 85/50. Old then new ECG:
Case 4: 40yo prior CABG with 2hr chest pain. AVSS. Old then new ECG:
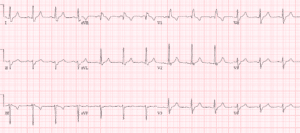
Case 5: 85yo with 2hrs chest pain. AVSS, no prior ECG
Case 6: 45yo with indigestion and diaphoresis. AVSS, no prior ECG
Case 7: 65yo with one day of constant pleuritic chest pain. Borderline tachy with normal BP/sats. No prior ECG
RBBB and Occlusion MI
When the right bundle branch is blocked, the septum depolarizes (left to right) followed by rapid depolarization of the left ventricle via the left bundle branch, and then the right ventricle depolarizes slowly. So QRS is prolonged >120ms (incomplete RBBB if <120ms), right-sided precordial leads have RsR’ in V1 (R from septal depolarization, S from LV depolarization, and R’ from delayed RV depolarization), and left-side precordial leads have RS wave (with rapid R from LV depolarization, and slurred S from slower RV depolarization). Axis should be normal in RBBB, and an abnormal axis could be the clue to a concomitant left anterior fascicular block (left axis, qR in I/aVL and rS in II/III/aVF) or left posterior fascicular block (right axis, rS in I/aVL, qR in III/aVF), or another reason for altered axis.
The right bundle runs down the interventricular septum and gets most of its blood supply from the LAD. So acute RBBB can develop if the septum is stretched by acute RV strain (from PE), or from acute coronary occlusion (especially of the LAD). RBBB in acute coronary occlusion can be pre-existing (more likely in older patients with comorbidities) or it can be acute, where it’s associated with larger infarcts, higher rates of heart failure and heart block, and higher mortality. While “new LBBB” is no longer considered a “STEMI equivalent”, there’s increasing recognition of the dangers of new RBBB in the context of acute coronary occlusion. Mortality from STEMI is higher in new RBBB compared to new LBBB, and higher still in bifascicular block—most commonly RBBB + LAFB, because of the left anterior fascicle is thinner and has more susceptible to ischemia than the left posterior fascicle [1]. While diffuse STD with reciprocal STE-aVR was once equated with left main occlusion, it’s now recognized to have a much broader differential diagnosis, but new RBBB+LAFB+STEMI has been associated with left main occlusion.[2]
As with other causes of abnormal depolarization, RBBB causes repolarization abnormalities that can mask or mimic ischemic changes (especially in right-sided precordial leads that have RSR’), but the concept of appropriate discordance can help. As a review summarized: “The major, terminal portion of the QRS complex and the initial portion of the ST segment/T wave are discordant, meaning that they are located on opposite sides of the isoelectric baseline. Thus, in the right to mid precordial leads, the largely positive QRS complex will be associated with ST-segment depression and an inverted T wave. A ‘violation’ of this concept will manifest as ST-segment elevation, which is concordant with the major, terminal portion of the QRS complex; the T-wave findings are often variable with either continued inversion or disappearance (lost within the greater ST segment itself). Anterior wall STEMI is therefore usually quite obvious if the clinician is comfortable with the appropriate appearance of the ST segment in RBBB.”[3] But sometimes ECG changes can be subtle or non-existent. As with the guideline for PCI in patients with refractory ischemia, the 2017 European Society of Cardiology advises, “Patients with MI and right bundle branch block (RBBB) have a poor prognosis. It may be difficult to detect transmural ischaemia in patients with chest pain and RBBB. Therefore, a primary PCI strategy (emergent coronary angiography and PCI if indicated) should be considered when persistent ischaemic symptoms occur in the presence of RBBB.”[4]
Back to the cases
Case 1: unnecessary cath lab activation
Old RBBB+LAFB, new rapid atrial fibrillation and rate-related ST changes. Cath lab activated based on mild inferior ST elevation, but ST changes resolved with rate control. Mild troponin elevation from non-occlusive MI.
Patient 2: unnecessary cath lab activation
There is old LAFB and new RBBB which was misinterpreted as showing anterior ST elevation, but this is within the prolonged depolarization of RBBB
Patient 3: LAD occlusion, delayed cath lab activation
New RBBB+LAFB + hyperacute T waves in V4-5 initially missed. A repeat ECG was done an hour later, now showing ST elevation V2-4 and I/AVL with reciprocal inferior ST depression, and cath lab activated. Proximal LAD occlusion, arrested in cath lab.
Patient 4: diagonal occlusion, rapid cath lab activation
There is old RBBB/LPFB with new ST elevation and pseudonormalized T waves in I/aVL, with reciprocal inferior ST depression. Cath lab activated: occlusion of graft to diagonal artery.
Patient 5: LAD occlusion, serial ECG then cath lab activation
First degree heart block and RBBB/LAFB unknown age. V2 has RBBB depolarization changes and should have discordant ST depression but instead there is mild concordant ST elevation.
Repeat ECG:
Now there is ST elevation in V2-3 and hyperacute T waves in V4-5. Cath lab activated: LAD occlusion.
Patient 6: posterior MI, rapid cath lab activation
Incomplete RBBB and LAFB age indeterminate. V3-4 have ST depression and T wave inversion (and V3 has no RSR’ so this is not simply discordant changes), and there is inferior ST depression and T wave inversion (reciprocal to the electrocardiographically silent lateral wall). 15 lead ECG:
Only minimal ST elevation in V8, but 12 lead shows posterior occlusion MI until proven otherwise. Cath lab activated: occluded obtuse marginal branch of circumflex. Discharge diagnosis “NSTEMI”. Normalizing ST/T on discharge ECG:
Patient 7: occlusion MI with atypical symptoms and no diagnostic ECG changes
Pleuritic chest pain with sinus tach, RBBB, S1Q3T3. While awaiting CT chest to rule out PE, troponin came back at 10,000, with ongoing chest pain. Cath lab activated: RCA occlusion. Discharge diagnosis “STEMI”.
Take home points on RBBB and Occlusion MI
- RBBB is a high risk feature in occlusion MI, especially if new and accompanied by LAFB. If a patient has ischemic symptoms and RBBB, compare with prior to see if this is new, and look for associated fascicular blocks and ST changes
- Anterior leads with RSR’ should have discordant ST/T changes, so concordant elevation or excessively discordant depression can be a sign of occlusion, while other leads will not have repolarization abnormalities. Finding the end of the QRS can identify ST changes.
References for ECG Cases 11: RBBB + Occlusion MI
- Neumann JT, Sorensen NA, Rubsamen N, et al. Right bundle branch block in patients with suspected myocardial infarction. Eur Heart J Acute Cardiovasc Care 2019 Mar;8(2):161-166
- Widimsky P, ROhac F, Stasek J, et al. Primary angioplasty in acute myocardial infarction with right bundle branch block: should new onset right bundle branch block be added to future guidelines as an indication for reperfusion therapy? Eur Heart J 2012 Jan;33(1):86-95
- Horton CL and Brady JB. Right bundle branch block in acute coronary syndrome: diagnostic and therapeutic implications for the emergency physician. Am J Emerg Med 2009 Nov;27(9):1130-41.
- Ibanez B, James S, Agewall S. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2018 Jan;39(2):119-177



















RBBB
present without ischemic symtom nerds any further investigation?
RBBB is often incidental, and if unrelated to the presentation (including ACS, PE, bifascicular block with syncope) does not require further investigations in ED. But in the outpatient setting the ACC recommend echo: “Patients may often be asymptomatic, particularly in the setting of isolated right bundle branch block (RBBB) or fascicular block…Cohort studies have generally demonstrated an association between LBBB, but not RBBB, presence and the development of coronary disease and heart failure…Patients with RBBB or intraventricular conduction delay on ECG also have increased risk of left ventricular systolic dysfunction compared with those with completely normal ECGs, yet the yield is lower than those patients with LBBB. Echocardiography can identify various structural cardiac abnormalities underlying conduction disturbance, including cardiomyopathy, valvular heart disease, congenital anomalies, tumors, infections, infiltrative processes,immunologically mediated conditions, and diseases of the great vessels and pericardium” (https://www.onlinejacc.org/content/accj/74/7/e51.full.pdf)
Thanks for sharing ????
Extremely helpful! Thank you for a large number of cases which include the the prior EKGs.