Topics in this EM Quick Hits podcast
Arun Sayal on nuances for assessment of scaphoid fractures (0:52)
Justin Morgenstern on the TTM2 trial and temperature management after cardiac arrest (7:42)
Sarah Reid on HEADS-ED screening tool for pediatric mental health (12:48)
Andrew Petrosoniak on pelvic binders and fracture tips (18:54)
Michelle Klaiman on what you need to know about kratom (24:43)
Anand Swaminathan on why femoral lines have made a come back and procedural tips (30:09)
Podcast production, editing and sound design by Anton Helman
Podcast content, written summary & blog post by Raymond Cho & Anton Helman
Cite this podcast as: Helman, A. Sayal, A. Swaminathan, A. Klaiman, M. Reid, S. Petrosoniak, A, Morgenstern J. EM Quick Hits 30 – Scaphoid Fracture, Therapeutic Hypothermia, HEADS-ED, Pelvic Trauma, Kratom, Femoral Lines. Emergency Medicine Cases. July, 2021. https://emergencymedicinecases.com/em-quick-hits-july-2021/. Accessed [date]
Scaphoid fractures: nuances of assessment
Epidemiology is important for pre-test probability assessment
- carpal injuries represent 20% of wrist injuries in the ED, of which 70% are scaphoid fractures
- Less likely in children < 15-years-old and adults > 50-years-old
- 20-30% of fractures are occult on initial X-rays
Diagnostic usefulness of the 3 physical exam maneuvers for scaphoid fractures
- Snuff box tenderness
- Poor specificity: many patients have physiologic snuff box tenderness at baseline; tip – palpate for asymmetric snuff box tenderness (i.e. check the contralateral wrist)
- Examination should be done with the wrist in ulnar deviation to expose the scaphoid

Palpate the snuffbox with the wrist in ulnar deviation to expose the scaphoid bone and compare to the contralateral wrist
- Palmar scaphoid palpation – tenderness at base of the thenar eminence over the palpable scaphoid tubercle with the wrist in radial deviation

Palmar location of scaphoid bone brought out by putting the wrist in radial deviation
- Axial thumb loading of 1st metacarpal to compress the scaphoid is less specific in elderly as a positive test is more likely indicative of CMC osteoarthritis rather than scaphoid fracture
- 3 of 3 portends a 70-90% likelihood of a scaphoid fracture (30-50% likelihood if 1/3).
- Consider adding dedicated scaphoid view if any one of the 3 exam maneuvers are positive
- Clamp sign has a pooled +LR of 8.6 for a scaphoid fracture. Ask the patient exactly where it hurts the most. If they place their thumb and index finger like a clamp on the volar and dorsal aspects of the base of the thumb, they have a positive Clamp Sign

The Clamp Sign has high positive likelihood ratio for the diagnosis of scaphoid fracture. Ask the patient to show you where the pain is the greatest. Grasping their scaphoid with their thumb and index finger is a positive Clamp Sign.
-
Duckworth AD, Jenkins PJ, Aitken SA, Clement ND, Court-Brown CM, McQueen MM. Scaphoid fracture epidemiology. J Trauma Acute Care Surg. 2012 Feb;72(2):E41-5
- Krastman P, Mathijssen NM, Bierma-Zeinstra SMA, Kraan G, Runhaar J. Diagnostic accuracy of history taking, physical examination and imaging for phalangeal, metacarpal and carpal fractures: a systematic review update. BMC Musculoskelet Disord. 2020 Jan 7;21(1):12.
- Ghane, M. R., Rezaee-Zavareh, M. S., Emami-Meibodi, M. K., & Dehghani, V. (2016). How Trustworthy Are Clinical Examinations and Plain Radiographs for Diagnosis of Scaphoid Fractures?. Trauma monthly, 21(5), e23345.
- Bäcker, H. C., Wu, C. H., & Strauch, R. J. (2019). Systematic review of diagnosis of clinically suspected scaphoid fractures. Journal of Wrist Surgery, 09(01), 081-089.
- Christopher R. C. et al. Adult Scaphoid Fracture. Academic Emergency Medicine, 2014; 21: 102– 121.
Temperature management after cardiac arrest – the TTM2 trial
Question: does targeted hypothermia (vs. controlled normothermia) impact all-cause mortality in patients with a coma following out-of-hospital cardiac arrest?
Design: international multi-center RCT of 1,900 patients randomized to a hypothermia (targeted temperature of 33°C) or controlled normothermia (targeted temperature of ≤ 37.5°C)
Primary outcome: all-cause mortality at 6 months
Results
- No difference in all-cause mortality at 6 months
- No difference in secondary outcomes including functional and neurologic outcomes
- Adverse events higher in hypothermia group, mostly dysrhythmias
Problems with this study: there was no true control group i.e., group that had no temperature control, and so this study does not address the utility of fever control. There is no conclusive evidence that fever control improves outcomes, but many clinicians still use this hypothesis in their practice.
Conclusions
- Therapeutic hypothermia (33°C) in patients with coma following an out-of-hospital cardiac arrest does not improve mortality, functional or neurologic outcomes and are associated with more adverse events
- Fever control in these patients is a reasonable hypothesis but there is no evidence to support this practice either
- Dankiewicz, J., Cronberg, T., Lilja, G., Jakobsen, J., Levin, H., Ullen, S., Rylander, C., Wise, M., Oddo, M., Cariou, A., Belohlavek, J., Hovdenes, J., et. al. (2021). Hypothermia versus Normothermia after Out-of-Hospital Cardiac Arrest. New England Journal of Medicine.
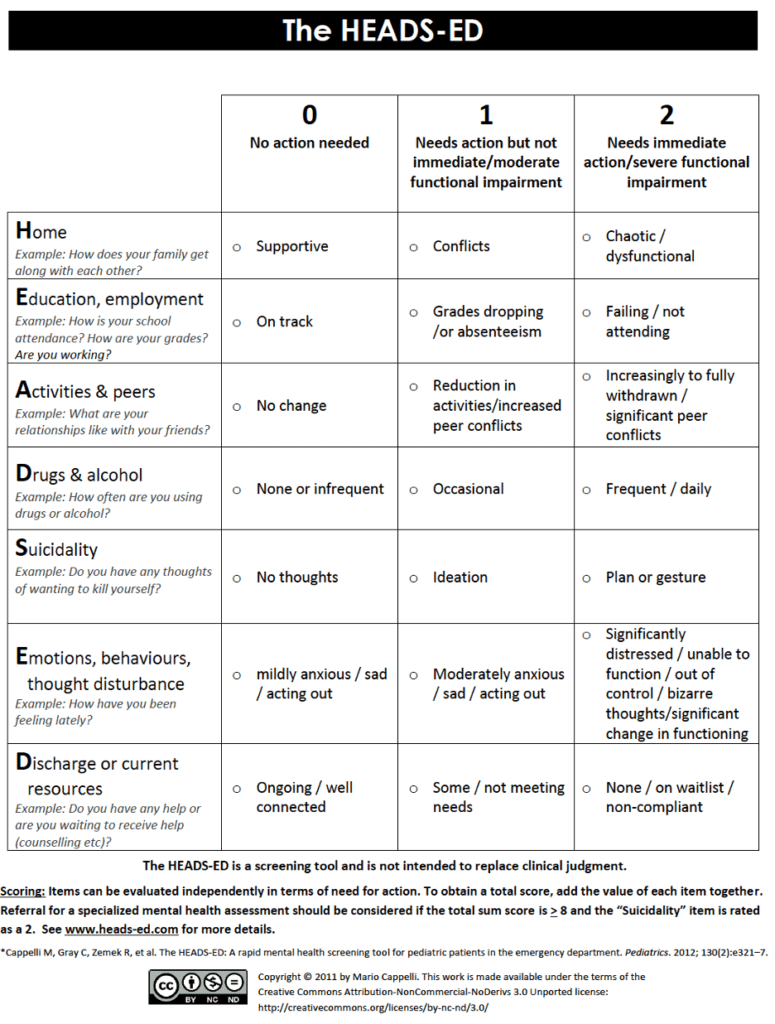
HEADS-ED pediatric and young adult rapid mental health screening tool
- HEADS-ED is a well-validated evidence-based rapid screening tool used to guide assessment in patients aged 6-25 years presenting to the ED with a mental health concern
- A score ≥8 or suicidality = 2 should prompt assessment by psychiatry team in the ED
- Cappelli, M., Zemek, R., Polihronis, C., Thibedeau, N. R., Kennedy, A., Gray, C., … Cloutier, P. (2020). The HEADS-ED: Evaluating the Clinical Use of a Brief, Action-Oriented, Pediatric Mental Health Screening Tool. Pediatr Emerg Care 2020 Jan;36(1):9-15.
- MacWilliams, K., Curran, J., Racek, J., Cloutier, P., & Cappelli, M. (2017). Barriers and Facilitators to Implementing the HEADS-ED: A Rapid Screening Tool for Pediatric Patients. Pediatr Emerg Care 2017 Dec;33(12):774-780.
- Cappelli, M., Gray, C.E., Zemek, R.L., Cloutier, P., Kennedy, A.M., Glennie, E., Doucet, G., & Lyons, J.S. (2012). The HEADS-ED: a rapid mental health screening tool for pediatric patients in the emergency department. Pediatrics 2012 Aug;130(2):e321-7.
- A Systematic Review of Instruments to Identify Mental Health and Substance Use Problems Among Children in the Emergency Department. Newton AS, Soleimani A, Kirkland SW, Gokiert RJ. Acad Emerg Med. 2017 May;24(5):552-568.
- Evaluating the HEADS-ED Screening Tool in a Hospital-Based Mental Health and Addictions Central Referral Intake System: A Prospective Cohort Study. Clark SE, Cloutier P, Polihronis C, Cappelli M. Hosp Pediatr. 2019 Feb;9(2):107-114.
- Emergency Department Screening for Adolescent Mental Health Disorders: The who, what, when, where, why, and how it could and should be done. Chun TH, Duffy SJ, Linakis JG. Clin Ped Emerg Med. 2013 March;14(1):3-11.
5 Tips for pelvic fractures and pelvic binder
1.Place the binder or sheet on the trauma bay stretcher before the patient is transferred onto it
2.Think of the pelvis as part of the circulation evaluation in your CABCs. Prioritize binding the pelvis early in the resuscitation of the polytrauma patient, usually prior to endotracheal intubation, if there is any suspicion that pelvic trauma is causing hemodynamic compromise. While binding the pelvis may not provide definitive source control, it may mitigate further movement and slow down bleeding from nearby vessels.
3.Think of the pelvic binder as a “trochanteric binder”; ensure the binder is centered over the greater trochanters, not high up on the pelvis over the ilium

Pelvic binder should be centered over the greater trochanters, not the ilium, for suspected or confirmed pelvic fracture with potential for hemorrhage
4.Do not log roll these patients the usual full 90 degrees lateral decubitus or rock the pelvis. There is a risk for increased hemorrhage and preventing clot formation by exacerbating pelvic instability when patients with unstable pelvic fractures are log rolled the usual full 90 degrees into lateral decubitus. Rather, turn the patient at most 10-20 degrees, just enough to visualize and palpate the back to assess for further injury.
5.If there are signs of pelvic trauma on exam or X-ray, do not forget to do a rectal/vaginal exam and insert a urethral catheter. The rectal/vaginal exam may reveal an open fracture and the catheter may reveal a bladder injury; gross hematuria may require a CT cystogram.
Do’s and Don’t of binding the pelvis from Episode 119 – Trauma: The First & Last 15 Minutes Part 2
- Helman, A. Bosman, K. Hicks, C. Petrosoniak, A. Trauma – The First and Last 15 Minutes Part 2. Emergency Medicine Cases. January, 2019. https://emergencymedicinecases.com/trauma-first-last-15-minutes-part-2. Accessed July 6, 2021.
- Hsu SD, Chen CJ, Chou YC, Wang SH, Chan DC. Effect of Early Pelvic Binder Use in the Emergency Management of Suspected Pelvic Trauma: A Retrospective Cohort Study. Int J Environ Res Public Health. 2017;14(10):1217.
- Coccolini F, Stahel PF, Montori G, et al. Pelvic trauma: WSES classification and guidelines. World J Emerg Surg. 2017;12:5.
Kratom – how to recognize and manage overdose and withdrawal
Background
- Kratom leaves, grown in Southeast Asia, have been used in herbal medicine for centuries as a stimulant, analgesic and sedative for relaxation
- Kratom’s active ingredients bind to the mu opioid receptor and act as partial opioid agonists
- Kratom is available for purchase widely as a powder or capsule
- Patients use Kratom for various purposes including management of opioid withdrawal, but physical/psychologic dependence may develop quickly
Clinical presentation
- Kratom has an opioid-like effect when taken at higher doses (5-15 g), but also has a stimulant-like effect at lower doses (1-5 g)
- Onset of action is 5-10 minutes and has a short half-life, with withdrawal occurring after approximately 12 hours and lasting 4 days
Management is similar to that of traditional opioid agonists
- Withdrawal: buprenorphine up to 16 mg on day 1 or a microdosing protocol
- Overdose: naloxone
Opioid withdrawal management on EM Cases
- Stanciu CN, Gnanasegaram SA, Ahmed S, Penders T. Kratom Withdrawal: A Systematic Review with Case Series. J Psychoactive Drugs. 2019 Jan-Mar;51(1):12-18.
- Swogger MT, Walsh Z. Kratom use and mental health: A systematic review. Drug Alcohol Depend. 2018 Feb 1;183:134-140. doi: 10.1016/j.drugalcdep.2017.10.012. Epub 2017 Dec 7.
- Weiss ST, Douglas HE. Treatment of Kratom Withdrawal and Dependence With Buprenorphine/Naloxone: A Case Series and Systematic Literature Review. J Addict Med. 2021 Apr 1;15(2):167-172.
The evidence for safety of femoral lines and procedural tips for success
- As PoCUS became the standard-of-care for placing central lines, femoral lines fell out of favour for internal jugular lines due to its perceived lower risk of infection
- More recent evidence suggests that the rate of infection is not higher for femoral lines compared to neck lines
- Marik et. al. SR metanalysis 2012 – no difference in catheter-associated bloodstream infections among 3 central line sites
- Parienti et. al. RCT 2015 – femoral and IJ sites had more thrombosis and bloodstream infections than subclavian lines, but femoral and IJ complications were similar
- It is reasonable to consider femoral lines more often than in the past, as they usually take less time to perform, there is usually more space in the room for the provider to place the line (the head of the bed is usually a crowded space in a resuscitation) and they carry no risk of pneumothorax
- Tips for placing a femoral line
- Externally rotate the hip to improve separation between the femoral artery and vein
- Aim high in the groin around the inguinal ligament to ensure placement in the common femoral vein (rather than branches)
-
Marik, P. E., Flemmer, M., & Harrison, W. (2012). The risk of catheter-related bloodstream infection with femoral venous catheters as compared to subclavian and internal jugular venous catheters. Critical Care Medicine, 40(8), 2479-2485.
-
Parienti, J., Mongardon, N., Mégarbane, B., Mira, J., Kalfon, P., Gros, A., Marqué, S., Thuong, M., Pottier, V., Ramakers, M., Savary, B., Seguin, A., Valette, X., Terzi, N., Sauneuf, B., Cattoir, V., Mermel, L. A., & Du Cheyron, D. (2015). Intravascular complications of central venous catheterization by insertion site. New England Journal of Medicine, 373(13), 1220-1229.
None of the authors have any conflicts of interest to declare





I think one of the major issues with binders is the “Trochanter” terminology. They are hard to find sometimes in obese patients, or in patients with clothes / safety gear on.
I wonder if some of this stemmed from a historical aversion to intimate terminology
I simply teach to centre on the genitals. We know where they are, it’s pretty obvious. And it’s essentially the same level.
You should be able to perform a FAST with a binder. You should not be able to insert a catheter.
We did an audit. About 60% were seriously misplaced. We should be able to do better.