Dr. Andrew Arcand & Dr. Laura Tate discuss the key clinical pearls and pitfalls in the recognition and management of many apparently benign hand emergencies that have serious morbidity, including high pressure injection injury, flexor tenosynovitis, gamekeeper’s thumb (or skier’s thumb), fight bites, hook of the hammate fractures and many more important hand emergencies. Dr. Tate & Arcand answer such questions as: which lacerations require prophylactic antibiotics? Which hand lacerations do not require sutures? How is rotational deformity best tested for metacarpal fractures? What are the pearls of tendon repair? How do you test for instability when you suspect a Gamekeeper’s thumb? How is compartment syndrome of the hand different to compartment syndrome in the leg? What are Kanavel’s signs of tenosynovitis? How should felons be managed in the ED? What are the most common errors that plastic surgeons see ED docs make?
Written Summary and blog post by Clarie Heslop, edited by Anton Helman January, 2013
Cite this podcast as: Arcand, A, Tate, L, Helman, A. Hand Emergencies. Emergency Medicine Cases. January, 2013. https://emergencymedicinecases.com/episode-29-hand-emergencies/. Accessed [date].
Fight Bites & Boxer Fracture
Suspect a “fight bite” when there is a laceration over an MCP joint. 10% of “fight bites” develop septic arthritis; these injuries need prophylactic antibiotics. For metacarpal fractures, assess for rotation & compare to contralateral hand:
- Phalanxes should point to the scaphoid in a closed fist (image below, left), or
- Look head on at the fingertips for rotation of fingernails, or
- Looking for scissoring with MCP in flexion (image below, right).
Reduce if rotation is present!
Metacarpal Fracture Acceptable angulation
40° for 5th MC, 30° for 4th MC, 20° for 3rd MCP, and 10° for 2nd. Reduce if greater angulation is present.
Pearls for Boxer Fracture Reduction
- Provide good anesthesia (i.e. ulnar nerve block).
- Consider using finger-traps for traction. Reduce by pushing dorsally on the distal bone fragment while providing counter pressure on proximal fragment, and immobilize in position of safety (MCP 90′ flexion, IP extension).
- Early follow-up (
Tendon injuries
Have a high index of suspicion.
- Inspect & test function of tendon against minimal or no resistance.
- For <50% extensor tendon injury, a splint may be sufficient.
- Our experts suggest ED physicians may repair extensor tendons cut >50% if ends are easily visible and easily opposed.
- Use a single horizontal mattress suture and splint the hand.
- All flexor tendon and all complex extensor tendon injuries should be splinted and seen by plastics in
Skin Lacerations
Is suturing indicated? Simple hand lacerations Digital nerve block: Single palmar injection of 2-3mL of 1% xylocaine at the base of the digit just distal to the proximal skin crease. Irrigation: Use 19g needle with 35cc syringe to irrigate copiously with saline or even tap water, under pressure.
Gamekeeper’s Thumb or Skier’s Thumb
Mechanism: Valgus force to abducted thumb. Exam: point of maximal tenderness is usually over the volar/ ulnar aspect of 1st MCP. Pincer grasp often painful with partial tears.
- Assess stability by applying radial stress to the distal thumb while immobilizing the proximal thumb and compare to contralateral thumb.
If >30′ deviation, assume instability. Get an X-ray to rule out avulsion # of proximal phalanx. For a partial injury, a 6-week splint may heal the tendon, but a complete tear requires surgery, so surgical exploration is often necessary for cases where a partial tear cannot be confirmed. All patients should be placed in a thumb spica splint and seen early for follow up (7 days) as nonunion of a complete tear requires extensive reconstruction.
High Pressure Injection Injury
Injury Liquid under high pressure causes severe injury when injected into the hand by: 1) Direct dissection of tissue planes and tissue ischemia, 2) Cytotoxicity of materials, and 3) Possible secondary infections. These injuries can result in extensive damage and lead to amputation. Don’t be fooled: these can appear benign but pain, pallor, and edema progress like a hand “compartment syndrome”. If history suggests a high pressure injection, contact plastics urgently for definitive exploration and debridement. X-ray can help determine the extent of injury.
Flexor Tenosynovitis
4 cardinal signs (Kanavel signs):
- Finger held in slight flexion,
- Fusiform swelling of the digit,
- Tender along tendon sheath, &
- Pain with passive extension.
Time is key because adhesions can form and permanently disable the digit. These must be urgently evaluated by plastic surgery, treated with IV antibiotics, and often admitted for either close monitoring, or urgent surgical irrigation and drainage. Start antibiotics, splint and elevate the hand, and refer to plastics.
Hook of the Hamate Fracture
Mechanism – either FOOSH, or an impact of a club or racket forced into the palm. Hook of the hamate fractures may not be seen on usual Xray views of the hand. The “carpal view” (supinated lateral view) should be ordered if suspicious about this fracture, and/or if pain is felt over the hypothenar eminence.
Not all hamate fractures appear on Xray. Some need further imaging (CT), and nonunion is very common. Excision of the fracture fragment is often necessary if there is nonunion. If a fracture is seen, immobilize the hand (in a volar slab, with MCP joints in flexion) and refer for follow-up within 4 weeks.
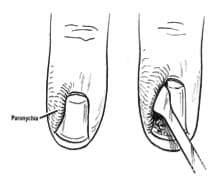
Paronychia
- Paronychia (nail edge infections, image at right) should be managed depending on the extent of the infection. A small infection without an abscess may improve with soaking the finger, and oral antibiotics.
- However, if an abscess has formed, it needs blunt dissection with a surgical blade, elevation of the lateral nail fold (image at right) and drainage of the sulcus between the lateral nail plate and the lateral epithelium.
- Irrigate copiously, and instruct the patient to soak the finger to keep the abscess open, or place a wick.
- If the abscess tracks under the nail, consider wedge resection of the nail plate, or nail plate removal if the entire nail plate is involved.
Felon
Compartments of the volar skin may form abscesses which need careful and thorough surgical decompression. See image (right). If urgent referral to a hand surgeon is not available, these must be managed in the ED. Cut and detach septae along whole length of distal phalanx nearest to the abscess site, releasing and irrigating very thoroughly. Avoid making incisions across the lateral aspect, to avoid injuring the digital nerve. After releasing all septae, swab, pack and treat with IV antibiotics, splinting, and elevation. Ensure urgent follow-up.
Tips for Hand Injuries
- When considering when to remove sutures in the hand, leave sutures that are over areas of tension (i.e. over a joint) for longer (at least 12 days) so they heal completely.
- If controlling bleeding is an issue, do NOT clamp any digital arteries, as the digital nerve is very nearby and hard to visualize. Use pressure, limited tourniquet and elevation to control bleeding safely.
- Prophylactic antibiotics are indicated for for all animal bites to the hand, and for certain complex injuries (crush wounds, wounds over a joint, or for immune compromised patients).
- If referring a hand abscess to a clinic, consider swabbing the drained fluid so MRSA status can be determined.
- Immobilizing the PIP joint in extension can stiffen the collateral ligaments causing permanent disability, so don’t splint PIP joint for greater than 1–2 weeks unless necessary, and if splinting, ensure an early referral time. (within 1–2 weeks).
Dr. Helman, Dr. Tate and Dr. Arcand have no conflicts of interest to declare.
For More on Hand Emergencies on EM Cases:
Best Case Ever 14: High Pressure Injection Injury
Episode 29b: Hand Emergencies Part 2
References
Friedrich, Jeffrey B., and Nicholas B. Vedder. “An evidence-based approach to metacarpal fractures.” Plastic and reconstructive surgery 126.6 (2010): 2205-2209. www.ncbi.nlm.nih.gov/pubmed/?term=Friedrich+JB%2…
Quinn, James, et al. “Suturing versus conservative management of lacerations of the hand: randomised controlled trial.” BMJ: British Medical Journal 325.7359 (2002): 299. www.ncbi.nlm.nih.gov/pubmed/?term=Quinn+J.+BMJ+2…
Smith III, Purcell, et al. “Excision of the hook of the hamate: a retrospective survey and review of the literature.” The Journal of hand surgery 13.4 (1988): 612-615. www.ncbi.nlm.nih.gov/pubmed/?term=Smith+P+et+al.…
Valente, Jonathan H., et al. “Wound irrigation in children: saline solution or tap water?.” Annals of emergency medicine 41.5 (2003): 609-616. www.ncbi.nlm.nih.gov/pubmed/?term=Valente%2C+JH.…













Thank you. Reference page 78, dealing with paronychia…how does one blunt dissect with a scalpel blade or sharp instrument?
Hi. Very late post, but a comment on the ebook chapter linked to this podcast: (pg62,EM Cases Digest, Vol 1 MSK and Trauma) please review the suggested test of the ulnar nerve at the hand. While I appreciate that there are various ways to test the peripheral nerves this test is more a test of median nerve function. Froments sign, for ulnar nerve function is similar but fundamentally different to the suggested position in the ebook. Thanks – I’m enjoying the read but found this a bit confusing.
Thanks for the correction David. I think the images were misplaced.
Excellent precise and concised article really i refreshed and add new tips to my experience about hand injuries