In this episode dedicated to emergency procedures pearls and pitfalls, tips and tricks, Dr. Jordan Chenkin & Dr. Jamie Blicker take us step by step through how best to perform surgical airways and pericardiocentesis, as well as place central lines and intraosseous lines. They explain the various methods for surgical airways including the bougie-assisted surgical airway. They review the indications, contraindications, and complications for all of these life saving procedures, and give us some amazing tips and tricks on what to do when things aren’t going as expected.
Written Summary & blog post by Claire Heslop, edited by Anton Helman February, 2013
Cite this podcast as: Chenkin, J, Blicker, J, Helman, A. Central Lines, Surgical Airways and Pericardiocentesis. Emergency Medicine Cases. February, 2013. https://emergencymedicinecases.com/episode-30-central-lines-surgical-airways-pericardiocentesis/. Accessed [date].
CENTRAL LINES
Are central lines the best option for fluid resuscitation? A wide bore short peripheral line has a faster flow rate than a central line. Triple-lumen catheters should not be chosen if rapid volume resuscitation is required; consider placing a sheath introducer.
Location Considerations: Choose the location you are most comfortable with, then consider the patient’s clinical scenario:
- For hypovolemic pts, think subclavian (doesn’t collapse as quickly),
- Coagulopathic – choose compressible site (femoral or IJ),
- Avoid sites with distorted anatomy or trauma proximal to the site (i.e. femoral is not a good choice for a patient bleeding in the abdomen).,
- For patients at high risk for pneumothorax, consider femoral
- Transvenous pacemaker insertion is easiest through right IJ, or left subclavian.
Catheter Related Bloodstream Infections
Risks are highest for lines inserted in very ill, crashing patients. Reduce the risk by using strict sterile technique! With strict technique, rates of infection may not be higher in the femoval site as previously thought. DVT risk is likely not higher in the femoral site. Antibioticimpregnated and heparin coated catheters also lower line infection rates.
The central line bundle reduces line infections, and should be used whenever possible, including a checklist and observer. Finally, use ultrasound guidance, as it has been proven to improve the chances of getting the line in on the first attempt which reduces complication rates.
Arterial Puncture during central line insertion
- Internal Jugular lines are associated with higher risk of arterial puncture compared to subclavian.
- U/S guidance reduces the risk, and for patients with IJ lying over the carotid artery, a lateral (posterior to the SCM) approach may be used.
- Confirm the catheter is in the vein directly with ultrasound, indirectly by a pressure transducer, by sending a VBG, or by shooting a CXR with the guidewire clamped at the skin. (If you do end up inserting a catheter into an artery, don’t remove it ! Call vascular surgery right away!)
Central Line Insertion in Coagulopathic Patients
- Choose a compressible site (femoral or IJ) and have the most experienced clinician with bedside ultrasound guidance to improve success on first puncture.
- The literature suggests there is no indication to correct a high INR or low platelets prior to placing a central line.
- A scalpel nick is not necessary for a triple lumen catheter,; the IJ is superficial and at risk of injury by the scalpel.
- Finally, consider using a peripheral catheter in the external jugular or IJ rather than a central line for these patients.
Landmarking for Central Lines
Blind landmarking may be necessary, if Ultrasound guidance is not available.
Femoral
If the artery cannot be felt, place a thumb on the pubic symphisis and index finger on ASIS, and use the apex of the V-shape of your 1st web space to find the femoral artery, then move 1cm medial at level of inguinal ligament. The optimal position is usually with the hip in external rotation & abducted.
Supraclavicular Subclavian
Use the “pocket shot” by inserting the needle 1cm lateral from the clavicular head of the SCM, and 1cm posterior to the clavicle. Aim toward contralateral nipple with needle 10% above horizontal.
Infraclavicular Subclavian
Aim below the clavicle, 1/3 from the medial head. Place a finger in the sternal notch and thumb at 1/3 along the clavicle, and insert the needle just lateral to the thumb at the pectoral triangle. Aim to have the needle just under the clavicle, under your thumb. Keep angle shallow.
Internal Jugular Central Line Procedure
Use Trendelenberg, with slight head rotation. Palpate the carotid pulse, and insert the needle lateral to carotid at the apex of the triangle formed by the 2 heads of the SCM.
Angle toward ipsilateral nipple, and when inserting the guidewire, use a low angle and watch the monitor during guidewire insertion.
Pearls & Pitfalls of Central Line Insertion
- Don’t insert the needle and sweep blindly for the vein; remove and reinsert if necessary.
- Double-check the guidewire is in the vein by U/S before dilating.
- Prep both IJ and SC on same side, in case another location needs to be attempted. (Don’t switch sides, and risk bilateral complications.)
- Try withdrawing the guidewire and rotating slightly if you have trouble advancing it.
How to Prevent an Air Embolism from Central Line Insertion
- Use Trendelenberg
- Occlude catheter hubs at all times and aspirate all air
- Insert on exhalation
Intraosseous Access
Consider an IO for any patients where IV access is anticipated to be difficult. Any medications and fluids that can go through the IV/CVC can be administered through the IO.* An IO is quicker and easier to place than an IV, and less training and experience is required. Pitfalls with insertion are usually due to errors in landmarking.
How accurate is the blood? Blood samples are accurate for Hb, Na, Cl, Gl, Cr and for crossmatch, but not for CO2 or potassium.
Where does the IO go? In kids, use the proximal tibia, and in adults the distal femur or proximal humerus may be preferable. Confirm placement by aspirating blood and flush the catheter over 8-10 seconds with 10-20mL of saline. Check that local compartment pressures are not increasing (which indicates leak into interstitium).
IO sites to avoid: Avoid broken bones, sites of previous IO attempt (fluid will leak), or sites near infections or previous surgeries. Discard the first few cc’s before sending bloodwork.
*Avoid calcium after ceftriaxone.
Update 2015: For more on intraosseous line placement see Episode 61 with Paul Hannam from Whistler’s Update in EM Conference
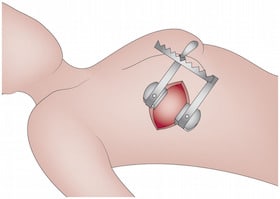
SURGICAL AIRWAYS
Approx. 1% of intubations in the ED are surgical airways; most are in the setting of trauma. The procedure for traditional surgical cricothyrotomy uses the following basic techniques.
1) Landmark: Palpate the cricothyroid membrane between the thyroid cartilage and the cricoid cartilage (approx 4 fingers above the sternal notch).
2) Stabilize the larynx with your nondominant hand throughout the procedure. Insert an 18g needle through the skin and pull back until air enters the syringe. Leave needle in to landmark.
3) Make a vertical skin incision 2cm long from bottom of cricoid to the thryroid cartilage to locate the cartilage and membrane.
4) Cut horizontally 1cm across the lower part of the membrane, and insert the tracheal hook (with upward traction).
5) Expand the hole with the dilator, and insert a #4 cuffed trach tube or a #6 cuffed ET tube along the dilator, then rotate 90 degrees. Don’t push the tube in more than ~5cm to avoid intubating R lung.
6) Confirm placement by usual methods + easy, smooth passing of NG tube through the tracheal tube.
Alternative Surgical Airway Methods
A bougie assisted technique (see video), with the tube passed over a bougie may be better for novice operators. A Seldinger guidewire technique may also be used.
- The “4-step technique” involving only 1 incision (horizontal) may be faster but has more bleeding complications.
Update 2015: Guidelines suggest that Bougie Assisted Cric favoured over Wire-guided Cric Here
Transtracheal Jet Ventilation
A large bore needle (12G or 14G) through the cricothyroid membrane, attached to a syringe and adapter, can oxygenate a patient for a brief period of time. This is a temporizing method, less reliable than surgical cric, and can only oxygenate, not ventilate.
PERICARDIOCENTESIS
Consider pericardial effusion with tamponade in any patient with unexplained SOB. Tamponade is a clinical diagnosis with ultrasound helping to confirm! Our experts recommend an apical approach, with U/S.
For apical pericardiocentesis, find a pocket of fluid on U/S closest to the probe with the patient in L lateral decubitus position. Use U/S to determine the distance from the skin to the fluid. For full details, please refer to the podcast audio, but our experts suggest the following tips:
- Once blood is aspirated, inject agitated saline under U/S guidance to confirm the needle is in the pericardium.
- Avoid positive pressure ventilation if possible in the patient who is crashing from tamponade, as it may worsen the tamponade.
Dr. Helman, Dr. Chenkin and Dr. Blicker have no conflicts of interest to declare.
For More on Central Lines, Surgical Airways and Pericardiocentesis on EM Cases:
Best Case Ever 15: Right Sided Thoracotomy
Best Case Ever 31: Emergency Pericardiocentesis
References
ACP Journal Club. Review: femoral and subclavian or internal jugular venous catheters do not differ for bloodstream infections. Whalen F et al. Ann Intern Med. (2012) www.ncbi.nlm.nih.gov/pubmed/23165684
Baombe, J. P., and B. A. Foëx. “Towards evidence based emergency medicine: Best BETs from the Manchester Royal Infirmary. BET 2: Intraosseous access and drug administration in adult cardiac arrest.” Emergency medicine journal: EMJ 28.6 (2011): 534-535. https://www.ncbi.nlm.nih.gov/m/pubmed/21602171/?…
Berenholtz et al. NEJM 2004;32:2014.
Ge, Xiaoli, et al. “Central venous access sites for the prevention of venous thrombosis, stenosis and infection.” Cochrane Database Syst Rev 3 (2012). www.ncbi.nlm.nih.gov/pubmed/22419292
LeMaster, Christopher H., et al. “Infection and natural history of emergency department–placed central venous catheters.” Annals of emergency medicine 56.5 (2010): 492-497. www.ncbi.nlm.nih.gov/pubmed/?term=Reid+C+et+al.+…
LeMaster, Christopher H., et al. “Infection and natural history of emergency department–placed central venous catheters.” Annals of emergency medicine 56.5 (2010): 492-497. www.ncbi.nlm.nih.gov/pubmed/?term=Reid+C+et+al.+…
Werner, Sandra L., Robert A. Jones, and Charles L. Emerman. “Effect of hip abduction and external rotation on femoral vein exposure for possible cannulation.” The Journal of emergency medicine 35.1 (2008): 73-75. www.ncbi.nlm.nih.gov/pubmed/?term=Werner+SL+et+a…
Curtis, Keith, et al. “Ultrasound‐guided, Bougie‐assisted Cricothyroidotomy: A Description of a Novel Technique in Cadaveric Models.” Academic Emergency Medicine 19.7 (2012): 876-879. www.ncbi.nlm.nih.gov/pubmed/?term=Curtis+K+et+al…
Hill, Chandler, et al. “Cricothyrotomy technique using gum elastic bougie is faster than standard technique: a study of emergency medicine residents and medical students in an animal lab.” Academic Emergency Medicine 17.6 (2010): 666-669. www.ncbi.nlm.nih.gov/pubmed/?term=Hill+C+et+al.+…
Hubble, Michael W., et al. “A meta-analysis of prehospital airway control techniques part II: alternative airway devices and cricothyrotomy success rates.” Prehospital Emergency Care 14.4 (2010): 515-530. www.ncbi.nlm.nih.gov/pubmed/?term=Hubble+MW+et+a…
Tsang, Teresa SM, et al. “Consecutive 1127 therapeutic echocardiographically guided pericardiocenteses: clinical profile, practice patterns, and outcomes spanning 21 years.” Mayo Clinic Proceedings. Vol. 77. No. 5. Elsevier, 2002. www.ncbi.nlm.nih.gov/pubmed/?term=Tsang+TS+et+al…






Leave A Comment