In this first part of our 2-part podcast on DKA and HHS, Drs Melanie Baimel, Bourke Tillmann and Leeor Sommer discuss the importance of identifying the underlying cause or trigger in DKA patients, the pitfall of ruling out DKA in patients with normal pH or normal serum glucose, how to close the gap effectively, why stopping the insulin infusion is almost never indicated, how to avoid cardiac collapse when DKA patients require endotracheal intubation, the best alternatives to plastic in the trachea, why using a protocol improves patient outcomes, how to avoid the common complications of hypoglycemia and hypokalemia, and much more…
Podcast voice editing by Raymond Cho. Production, sound design & editing by Anton Helman.
Written Summary and blog post by Lorraine Lau & Winny Li, edited by Anton Helman September, 2020.
Cite this podcast as: Helman, A. Baimel, M. Sommer, L. Tillmann, B. Episode 146 – DKA Recognition and ED Management. Emergency Medicine Cases. September, 2020. https://emergencymedicinecases.com/dka-recognition-ed-management. Accessed [date].
The Difficulty in Diagnosing Diabetic Ketoacidosis (DKA)
There are no definitive criteria for the diagnosis of DKA according to the 2018 Canadian DKA Guidelines. As such, it is important to have a low threshold to consider the diagnosis in any diabetic patient who presents with polyuria, polydipsia, hyperpnea, abdominal pain/nausea/vomiting or altered level of awareness. While most patients with DKA will have the triad of hyperglycemia, anion gap metabolic acidosis and ketonemia, there are important exceptions:
- DKA patients can have a normal glucose (euglycemic DKA – see below)
- DKA patients can have a normal pH and a normal bicarbonate (normal VBG) in the context of ketoacidosis plus metabolic alkalosis as a result of vomiting and/or the triggering illness
- Negative urine ketones should not be used to rule out DKA, as urine tests measure the presence of acetoacetate, but not β-hydroxybutyrate
A β-hydroxybutyrate level > 1.5 mmol/L has a sensitivity of 98-100% and specificity of 78.6-93.3% for the diagnosis of DKA in diabetic patients presenting to the ED with elevated serum glucose levels.
Clinical Pearl: Many patients with DKA present with some degree of abdominal pain. Severe abdominal pain with only mild ketoacidosis argues against DKA as the cause. When in doubt about the need for an abdominal imaging, resuscitate the patient first, and perform serial abdominal examinations. Have a low threshold to image if the ketoacidosis improves but the patient continues to be symptomatic or clinically worsens.
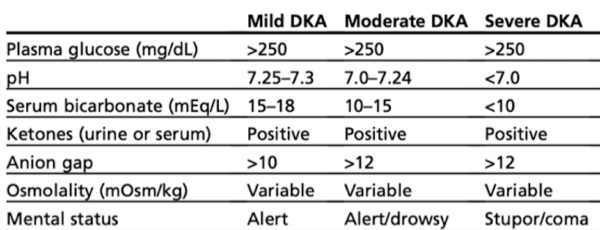
Severity categorization of DKA
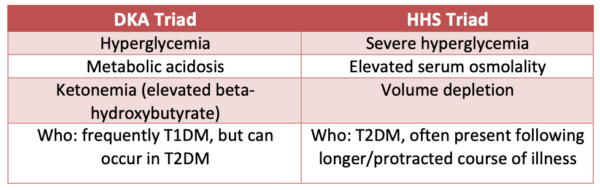
Differentiating DKA from Hyperglycemic Hyperosmolar Syndrome (HHS)
DKA and HHS may occur concurrently.
Evaluation for precipitating cause of DKA is paramount as it is often the cause of of death in patients with DKA
DKA can be the initial manifestation of diabetes, but it often occurs in the context of known diabetes plus a trigger. Most often, it is due to medication non-adherence, incorrect dosing or infection. However, any physiologic stress can trigger DKA.
Common causes include “The 5 I’s”:
- Infection (pneumonia, UTI, skin, abdominal)
- Infraction (MI, stroke, bowel infarction)
- Infant on board (pregnancy)
- Indiscretion (dietary nonadherence)
- Insulin deficiency (insulin pump failure or nonadherence)
In addition, common drugs that can trigger DKA include glucocorticoids, diuretics and atypical antipsychotics.
DKA lab work-up
DKA work-up should include CBC, electrolytes, extended electrolytes, creatinine, BUN, albumin, VBG, lactate, serum ketones, as well as consideration for:
- BhCG (pregnancy may be a trigger of DKA)
- ECG/Trop (only if ischemia suggested in history)
- Cultures, UA etc. for suspected infection trigger
- β-hydroxybutyrate if diagnosis unclear
Lactate is a potentially important prognostic factor in predicting the severity of DKA and in monitoring the progression or resolution.
Acid-base disturbances in DKA
DKA patients classically have an anion-gap metabolic acidosis due to lipolysis and an accumulation of ketoacids. However, diabetic patients with significant GI loss can have a normal pH or alkalemia because of a mixed acid-base disturbance.
In such cases, use the Simplified Stewart Approach:
Base-excess =
Other ions = Base excess − [Na−Cl–35] – [1–lactate] – [0.25 x (42−albumin)]
Other ions =
Base excess − [Na−Cl–35] + [1–lactate] + [0.25 x (42−albumin)] If the major determinants of acid-base do not explain the base deficit, then there are unmeasured ions present.
Pitfall: Avoid ruling out DKA based on a normal or near normal VBG. DKA patients can have a normal pH due to the underlying trigger of the DKA contributing to a mixed acid-base picture.
Sorting out ketonemia: The differential diagnosis of ketoacidosis
The differential diagnosis for ketoacidosis includes:
- DKA
- Alcoholic ketoacidosis
- Starvation ketosis
- Isopropyl alcohol ingestion
In the presence of low or normal glucose levels, it is less likely that it is DKA. You can have positive serum ketones and anion gap metabolic acidosis with alcoholic ketoacidosis and starvation ketoacidosis, and these may be difficult to distinguish clinically. Starvation ketosis responds quickly to glucose and the acidosis is generally less severe. The clinical history will be key in identifying the diagnosis.
Euglycemic DKA
Euglycemic DKA involves a relative carbohydrate deficiency state/normalization of serum glucose and concomitant elevation of counter-regulatory stress hormones that leads to free fatty acid catabolism and ketone production.
Maintain a high index of suspicion for DKA in the following patients who present with nausea, vomiting, shortness of breath and/or metabolic acidosis, and evaluate for DKA with serum ketones and/or β-hydroxybutyrate:
- T1/T2DM Patients taking SGLT-2 inhibitors (the “zins”)
- Pregnant patients – due to transplacental glucose transport, will have relative euglycemia (more common in second or third trimester)
- Chronic pancreatitis
- Bariatric surgery patients – due to absorption issues
For management of euglycemic DKA, you may need to start fluids with dextrose sooner in the treatment process.
Walter Himmel’s Best Case Ever on Euglycemic DKA
ED Management of DKA
Goals of treatment in DKA
The initial goals of treatment in patients with DKA include:
- Correction of fluid deficits
- Replacement of potassium
- Stopping ketone production by closing the anion gap with insulin
- Treating underlying precipitant
Essential concept in the ED management of DKA: The focus is not on lowering the glucose, but rather closing the gap
DKA is not an issue of hyperglycemia per se, but rather an excess in serum ketone production due to low circulating levels of insulin. The cornerstone of DKA treatment is the correction of metabolic homeostasis by reducing ketone production via insulin and not the correction of hyperglycemia.
Using standardized DKA order sets for the management of DKA has been shown to decrease the time to anion gap closure, reduce length of stay in hospital, and minimize complications during treatment.

2018 Canadian Diabetes Association DKA Guidelines treatment algorithm, adapted from https://guidelines.diabetes.ca/docs/CPG-2018-full-EN.pdf
DKA Fluid Resuscitation
Osmotic diuresis from hyperglycemia results in significant volume depletion. Fluid resuscitation will help restore intravascular volume, achieve normal tonicity, improves organ perfusion, decreases lactate formation, improves renal function.
- Use NS or RL for initial fluid replacement (American Diabetes Association -ADA): 1000-1500mL NS over 1 hr) then adjust to patient’s hemodynamic and electrolytes status, and maintain between 250 and 500 mL/hr
- ADA: Patients with a normal or high corrected sodium concentration can be switched to 0.45% sodium chloride after the first hour of fluid replacement
- Add dextrose (D5W) to the IV fluid if/when blood glucose approaches normal to allow continued insulin infusion at a rate sufficient to resolve DKA while avoiding hypoglycemia OR when glucose <15 (250-300mg/DL) switch to D5-1/2NS NS at an initial rate of 150 to 250 mL/h
- Our experts recommend starting with NS or RL and consider ongoing fluid resuscitation with RL to avoid the hyperchloremic acidosis associated with large volumes of NS
Key point: Volume resuscitation must precede insulin therapy in order to adequately restore intravascular volume and tonicity. Early insulin therapy has the added risk of hypoglycemia and hypokalemia.
The 2-bag method of fluid management in DKA
Two bags of half NS, one with and one without 10% dextrose (D10W) are adjusted on the basis of hourly blood glucose monitoring to maintain an IV fluid rate of 250 mL/h. Two retrospective studies of more than 500 patients found that the 2-bag method was associated with earlier correction of acidosis and shorter duration of IV insulin compared with conventional delivery of IV fluids. Use of the 2-bag method in the ED may reduce the need for hospital admission, and it may be associated with less hypoglycemia compared with conventional treatment.
DKA Insulin Therapy: Closing the Gap
Again, the primary problem in patients with DKA is ketoacidosis (not hyperglycemia). Our overall goal is to titrate insulin to treat the ketoacidosis and close the gap. Glucose levels are used as a surrogate measurement of the efficacy of insulin therapy. Supplemental glucose should be provided as glucose approaches normal to allow for continued insulin therapy to resolve the ketoacidosis while avoiding hypoglycemia.
- Start short-acting insulin at a fixed weight-based dosing of 0.1U/kg/hr
- Target blood glucose of 12-14mmol/L and normalization of the anion gap
- When blood glucose <14mmol/L, add dextrose D5 infusion to prevent hypoglycemia while continuing insulin infusion
- If glucose falls < 4mmol/L, do not stop insulin infusion, but decrease by 50% (no less than 0.05U/kg/hr), provide 1 amp of D50 and switch dextrose infusion from D5 to D10
Patients should also be allowed to eat if it is deemed safe to do so. There is no evidence to support keeping the patient NPO.
Common pitfall: A common pitfall is stopping the insulin infusion when the glucose normalizes or falls below normal the normal limit. Do not stop the insulin infusion when serum glucose normalizes or is low. The patient will very quickly become ketotic again as insulin is required to shut off the underlying metabolic derangement of ketoacidosis.
What about insulin bolus? There is no role for bolus dosing of insulin, except possibly in the peri-arrest situation. Bolus insulin increases the risk of hypoglycemic events, prolonged gap closure, and longer hospital stays.
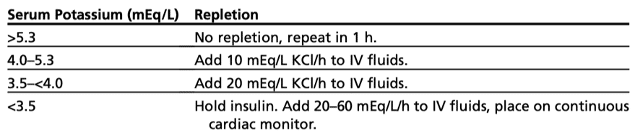
Hypokalemia: A Common Complication of DKA
Patients with DKA have large total body potassium deficits. However, the initial potassium reading is commonly normal or high due to intracellular shifts secondary to volume contraction and metabolic acidosis. Potassium must be replaced prior to initiation of insulin therapy as insulin further promotes an intracellular shift of potassium.
If the patient can tolerate oral potassium replacement, it is preferred over the IV route as it thought to have better systemic absorption.
Starting Long-acting Insulin in the ED
Long-acting insulin should be considered early (well in advance of discontinuing the infusion), even in the ED. Early initiation of long-acting insulin facilitates transitioning off the insulin infusion, reduces the incidence of hyperglycemia, and may decrease hospital length of stay.
Patients can generally be treated with their home insulin regimen (ideally a single daily dose of glargine). For a patient naive to insulin, a starting dose of 0.25 units/kg daily of glargine (Lantus) may be given.
Role of Bicarbonate in Severe DKA
The literature does not support replacing bicarb in adult DKA patients with pH ≥6.9. There is retrospective evidence of transient paradoxical worsening of ketosis and an increased need for potassium supplementation in patients who received bicarb. Our experts caution against the routine use of bicarbonate therapy in DKA. The decision to give bicarb should be tailored to the individual patient, their hemodynamics and their acid/base status.
Our experts recommend consideration for bicarbonate in the severe DKA patient just prior to endotracheal intubation, as it may help transiently buffer the pH against the rise in CO2 that occurs during induction +/- paralysis.
Troubleshooting: Anion Gap is not Closing
If the anion gap is not closing, consider the following possibilities:
- Inadequate fluid resuscitation
- Inadequate insulin dose
- Malfunction of insulin infusion
- Underlying diagnosis contributing to anion gap that has not been addressed
Interventions if the anion gap is not closing:
- Evaluate fluid status (e.g. with ultrasonography), provide additional crystalloid if necessary
- Consider increasing the insulin infusion rate (see next section)
- Re-evaluate for a missed underlying diagnosis
- Consider checking beta-hydroxybutyrate and lactate levels, to exclude an occult/worsening lactic acidosis
Learn more about using POCUS to guide fluid resuscitation at POCUS Cases 7 IVC Assessment of Volume Status
(Avoid) Intubating the DKA Patient
Patients with DKA are physiologically challenging patients to intubate for several reasons. Their respiratory dynamics of hyperpnea to correct their underlying metabolic acidosis means the ventilator must equally match their large tidal volume and respiratory rate. This intrinsically puts the patient at risk for ventilator induced lung injury and subsequent development of ARDS. Furthermore, these patients with profound metabolic acidosis are at risk of circulatory collapse peri-intubation as periods of apnea during intubation will cause their pCO2 levels to rise rapidly, worsening the acidosis.
If you must intubate:
- Resuscitate before you intubate
- Consider ketamine +/- paralytic; continue to bag if paralytic used to avoid any period of apnea
- Consider an antiemetic
- Consider giving IV bolus bicarb, especially if serum bicarb <10
- High tidal volume (8cc/kg) and RR (24-28) to hyperventilate
- Consider asking for additional help from your anesthesiology colleagues
The Role of NIPPV in DKA
Oxygenation is rarely an issue in DKA, but rather work of breathing and respiratory fatigue may occur. Our experts do not recommend the routine use of BiPAP in DKA patients given the risk of aspiration and emesis in these patients, as they often concurrently have gastroparesis. Only consider NIPPV if the patient is in a highly monitored setting with one-to-one nursing care.
A non-rebreather and/or high flow nasal cannula should be considered if there is a suspected primary hypoxic issue requiring supplemental oxygen.
Avoiding Cerebral Edema in DKA
The key to avoiding cerebral edema in the management of DKA is to go slow with resuscitation.
- Avoid over-aggressive fluid administration
- Do not drop the glucose too fast; avoid reducing the glucose below <200 mg/dL (<11.1 mmol)
- Replace fluids gradually
- Consider isotonic fluids (e.g. D5 RL can be used as a source of glucose-containing IV fluid, rather than hypotonic fluids such as D10W or D5 1/2 NS).
- Avoid lowering the serum osmolality by more than 3 mmol/kg/hour or decreasing sodium by >10 mmol/24 hours
- Note that the sodium will often initially increase during resuscitation due to glucose entering the cells. This does not reflect an increase in serum osmolality and does not require treatment with free water
- The best parameter to track is the measured or estimated serum osmolality
Criteria for resolution of DKA
Glucose <11.1 mmol (<200mg/dL) + 2 of:
- Normalization of AG
- Venous pH >7.3
- Serum bicarbonate ≥15mEq/L
Key take home points for ED management of DKA
- Identify the underlying cause/trigger which is often the cause of death in DKA and HHS patients – use the mnemonic 5 “I”s plus drugs if that helps you remember the triggers
- Do not rule out DKA based on a normal serum pH or a normal serum glucose – measure beta-hydroxybutyrate when in doubt
- Main goal in DKA is to close the gap, not normalize the glucose level
- Do not stop the insulin when serum glucose becomes normal or low; instead, give glucose
- Allow patient to eat as soon as there is no aspiration risk
- Avoid intubation and BiPAP whenever possible in severe DKA – HFNC is your go-to if they are not doing well on a non-rebreather
- Know how to differentiate all the causes of ketoacidosis – there are subtle clues
- Use a protocol – there is good evidence that protocols for DKA management improve patient outcomes
- Monitor carefully for complications of DKA: hypoglycemia, hypokalemia, ARDS
For part 2 of this series on Diabetic Emergencies go to Episode 147 HHS Recognition and ED Management
References
- Goguen J, et al. Hyperglycemic emergencies in adults: 2018 Clinical Practice Guidelines. Canadian Journal of Diabetes, 42: S109-S114.
- Kitabchi AE, Umpierrez GE, Miles JM, et al. Hyperglycemic crises in adult patients with diabetes. Diabetes Care. 2009;32(7):1335-1343.
- Wolfsdorf JI, Glaser N, Agus M, et al. ISPAD Clinical Practice Consensus Guidelines 2018: diabetic ketoacidosis and the hyperglycemic hyperosmolar state. Pediatr Diabetes. 2018;19 Suppl 27:155-177.Fayfman M, Pasquel F, Umpierrez G. Management of Hyperglycemic Crises: Diabetic Ketoacidosis and Hyperglycemic Hyperosmolar State. Med Clin North Am. 2017;101(3):587-606.
- Umpierrez G, Freire A. Abdominal pain in patients with hyperglycemic crises. J Crit Care. 2002;17(1):63-67.Sheikh-Ali M, Karon B, Basu A, et al. Can serum beta-hydroxybutyrate be used to diagnose diabetic ketoacidosis? Diabetes Care. 2008;31(4):643-647
- Goyal N, Miller JB, Sankey SS, et al. Utility of initial bolus insulin in the treatment of diabetic ketoacidosis. J Emerg Med. 2010;38(4):422-427.
- Ma OJ, Rush MD, Godfrey MM, et al. Arterial blood gas results rarely influence emergency physician management of patients with suspected diabetic ketoacidosis. Acad Emerg Med. 2003;10(8):836-841.
- Adrogué HJ, Barrero J, Eknoyan G. Salutary effects of modest fluid replacement in the treatment of adults with diabetic ketoacidosis. Use in patients without extreme volume deficit. JAMA. 1989;262(15):2108-2113.
- Semler MW, Self WH, Wanderer JP, et al. Balanced crystalloids versus saline in critically ill adults. N Engl J Med. 2018;378(9):829-839.
- Goldenberg RM, Berard LD, Cheng AYY, et al. SGLT2 inhibitor-associated diabetic ketoacidosis: clinical review and recommendations for prevention and diagnosis. Clin Ther. 2016;38(12):2654-2664.
- Chua HR, Schneider A, Bellomo R. Bicarbonate in diabetic ketoacidosis – a systematic review. Ann Intensive Care. 2011;1(1):23.
- Duhon B, Attridge RL, Franco-Martinez AC, et al. Intravenous sodium bicarbon- ate therapy in severely acidotic diabetic ketoacidosis. Ann Pharmacother 2013; 47(7–8):970–5.
- Van Ness-Otunnu R, Hack JB. Hyperglycemic crisis. J Emerg Med 2013;45(5): 797–805.
- Seheult J, Fitzpatrick G, Boran G. Lactic acidosis: an update. Clin Chem Lab Med. 2017;55(3):322-333.
- Thuzar M, Malabu UH, Tisdell B, Sangla KS. Use of a standardised diabetic ketoacidosis management protocol improved clinical outcomes. Diabetes Res Clin Pract 2014;104:e8-11. 10.1016/j. diabres.2014.01.016
- Kitabchi AE, Murphy MB, Spencer J, Matteri R, Karas J. Is a priming dose of insulin necessary in a low-dose insulin protocol for the treatment of diabetic ketoacidosis?Diabetes Care 2008;31:2081-5. 10.2337/dc08- 0509 pmid:18694978.
- Haas NL, Gianchandani RY, Gunnerson KJ, et al. The Two-Bag Method for Treatment of Diabetic Ketoacidosis in Adults. J Emerg Med 2018;54:593- 9. 10.1016/j.jemermed.2018.01.004.
- Munir I, Fargo R, Garrison R, et al. Comparison of a ‘two-bag system’ versus conventional treatment protocol (‘one-bag system’) in the management of diabetic ketoacidosis. BMJ Open Diabetes Res Care 2017;5:e000395. 10.1136/bmjdrc-2017-000395.
- Chua HR, Schneider A, Bellomo R. Bicarbonate in diabetic ketoacidosis – a systematic review. Ann Intensive Care 2011;1:23. 10.1186/2110-5820-1- 23 pmid:21906367.
Euglycemic DKA
- Peters AL, Buschur EO, Buse JB, Cohan P, Diner JC, Hirsch IB. Euglycemic Diabetic Ketoacidosis: A Potential Complication of Treatment With Sodium-Glucose Cotransporter 2 Inhibition. Diabetes Care. 2015;38(9):1687-93.
- Jazi M, Porfiris G. Euglycemic diabetic ketoacidosis in type 2 diabetes treated with a sodium-glucose cotransporter-2 inhibitor. Can Fam Physician. 2016;62(9):722-4.
- Munro JF, Campbell IW, McCuish AC, Duncan LJP. Euglycaemic diabetic ketoacidosis. BMJ 1973;2:578–580.
- Hine J, Paterson H, Abrol E, Russell-jones D, Herring R. SGLT inhibition and euglycaemic diabetic ketoacidosis. Lancet Diabetes Endocrinol. 2015;3(7):503-4.
- Rosenstock J, et al. Euglycemic Diabetic Ketoacidosis: A Predictable, Detectable, and Preventable Safety Concern With SGLT2 Inhibitors. Diabetes Care. 2015 Sep;38(9):1638-42.
Drs. Helman, Tillman, Baimel and Sommer have no conflicts of interest to declare
Now test your knowledge with a quiz.





Thank for a great podcast.
I would like to offer an alternative approach to management of DKA where we do not use use an insulin infusion at all.
We give 0.3 units/kg of Lantus + 0.3 units of Lispro at time of diagnosis. Measure glucose q2 for 4 hours. At 2 hour mark if glucose is still high we will give another dose of Lispro but at 0.2 units/kg.
We also use the 2 bag method where we start a D51/2NaCl + 20KCl maintenance infusion and LR for bolus and replacement fluid.
In this approach we have closed the gap just as fast as compared to insulin infusion and have lower incidence of hypoglycemia.
Question to the panel…
There is some evidence showing that kids who “develop” CE, ALREADY HAVE CE when we start treatment. The hypothesis is that kids brains have higher oxygen demand and develop global ischemia from hypo perfusion a lot faster than adult brains. Also, the profound vasoconstriction with high catecholamines and acidosis, together with blood-brain barrier dysfunction lead to inflammatory changes causing CE. Here: https://www.nejm.org/doi/full/10.1056/NEJM200101253440404
Another study (18 kids only) showed MRI was worse early in the severe DKA than after treatment: http://pediatrics.aappublications.org/content/131/1/e73?sso=1&sso_redirect_count=1&nfstatus=401&nftoken=00000000-0000-0000-0000-000000000000&nfstatusdescription=ERROR%3a+No+local+token
And finally… Canadians (yes, great Canadians) found the highest features associated with CE were high BUN, low CO2, and bicarb treatment, suggesting that severe dehydration/hypovolemia and acidosis are important risk factors. https://www.jpeds.com/article/S0022-3476(04)01216-8/fulltext
So… Going back to my question. What do I do for the shocky, Glasgow of 3, severe DKA kid? Do I correct hypovolemia? In my simple way of thinking, delaying intravascular volume repletion to 36 hrs, is delaying brain perfusion for 36 hr. There is now enough evidence to suggest that its not the treatment, but the ischemia and blood-brain barrier dysfunction what causes CE and by delaying adequate brain perfusion we may be putting these kids at risk. I think a larger trial of MRI pre and during treatment might be a better trial to answer the question. Do children with severe DKA already have CE prior to treatment?
OK.. rant over.
This is a review on pediatric DKA fluid management and cerebral edema in our EM Quick Hits by Sarah Reid….
“A practice changing PECARN study compared two fluid protocols in 1,389 cases of DKA
Fast protocol: 10 mL/kg bolus + 10 mL/kg bolus (both with NS) followed by replacement of a 10% fluid deficit + maintenance over 36 hours with either NS or 0.45 NS
Slow protocol: 10 mL/kg bolus (with NS) followed by replacement of a 5% fluid deficit + maintenance over 48 hours with either NS or 0.45 NS
No difference between the fluid protocols in worsening mental status, cerebral injury, or post-DKA cognitive function
Bottom line: we don’t have to be so judicious with fluids in pediatric DKA; it’s almost always safe to start your resuscitation with 10mL/kg NS bolus regardless of fluid status and repeat if still hypoperfused”
And here is the pediatric DKA algorithm that I recommend. Hope this helps clarify fluid management in pediatric DKA.
https://trekk.ca/system/assets/assets/attachments/349/original/2019-01-10_DKA_Algorithm_v_1.0.pdf
I haven’t treated a pediatric patient in about 6 years so by no means an expert in this area. I would agree with what Anton has posted above and defer to the NEJM PECARD study https://www.nejm.org/doi/full/10.1056/nejmoa1716816
Cerebral edema seems to be from the disease itself rather than the treatment. I would prioritize the treatment of shock.
Two review articles that summarize this well:
1) Cashen K, Petersen T. Diabetic Ketoacidosis. Pediatr Rev 2019 American Academy of Pediatrics;40(8):412-420.
2) Long B, Koyfman A. Emergency Medicine Myths: Cerebral Edema in Pediatric Diabetic Ketoacidosis and Intravenous Fluids. J Emerg Med 2017;53(2):212-221.
“Resuscitate before you irradiate!”
Is this part right? I mean it seams a bit fast as in my hospital we usually go very slow and awoid lowering the glucose more than 1mmol/hour (we don’t messure or calculate osmolality for some reason)
“Avoid lowering the serum osmolality by more than 3 mmol/kg/hour”
Very nice podcast. keep doing the good work.
Good podcast!