In this ECG Cases blog we look at 6 patients who presented with potentially ischemic symptoms, “STEMI negative” but signs of a specific coronary occlusion.
Written by Jesse McLaren; Peer Reviewed and edited by Anton Helman, May 2020
Six patients presented with ischemic symptoms, “STEMI negative”.
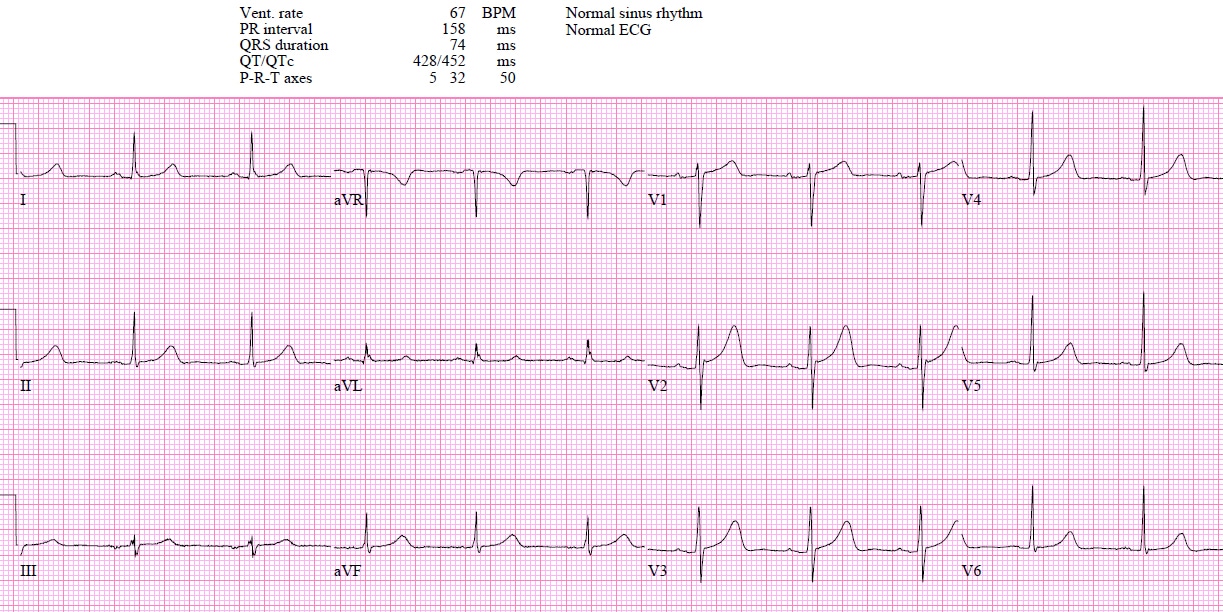
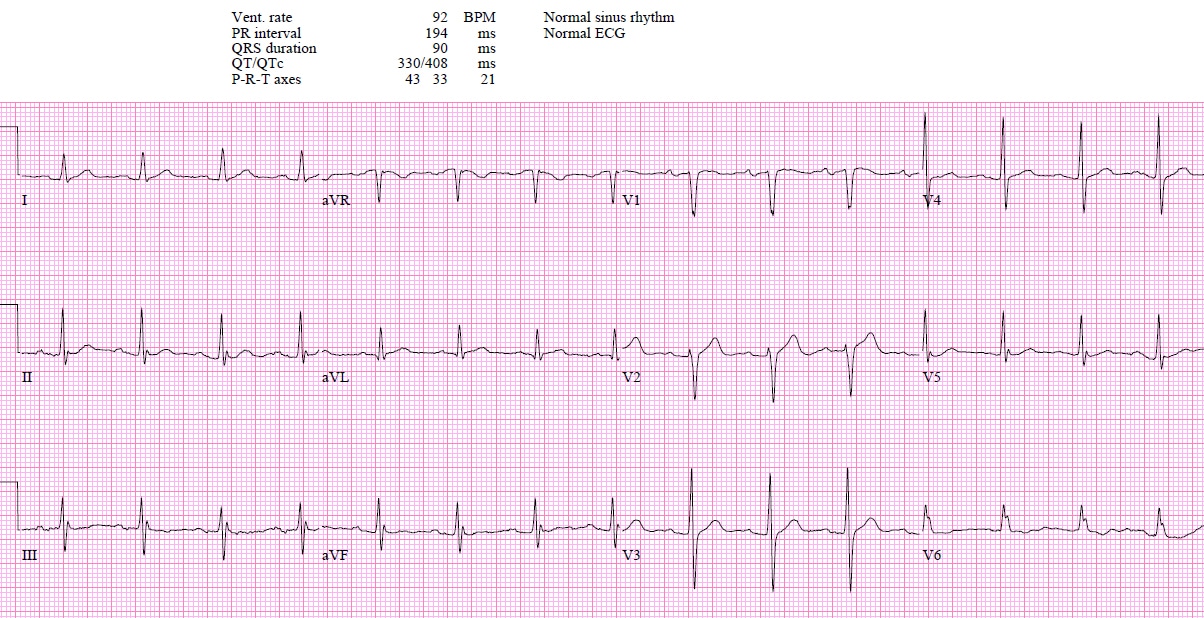
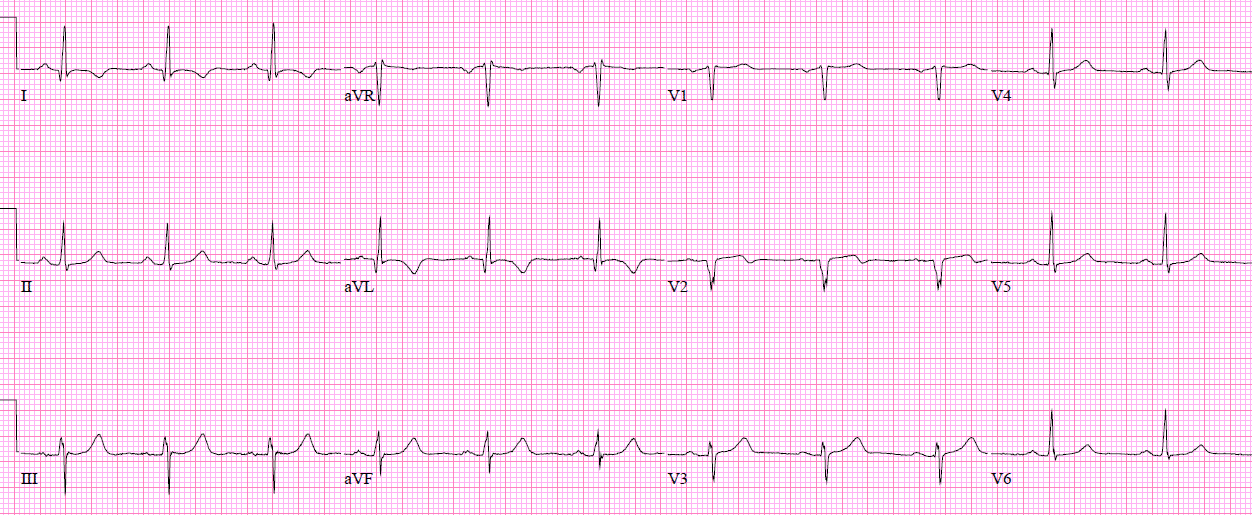
Patient 1: 50yo with 5 hours of chest pain
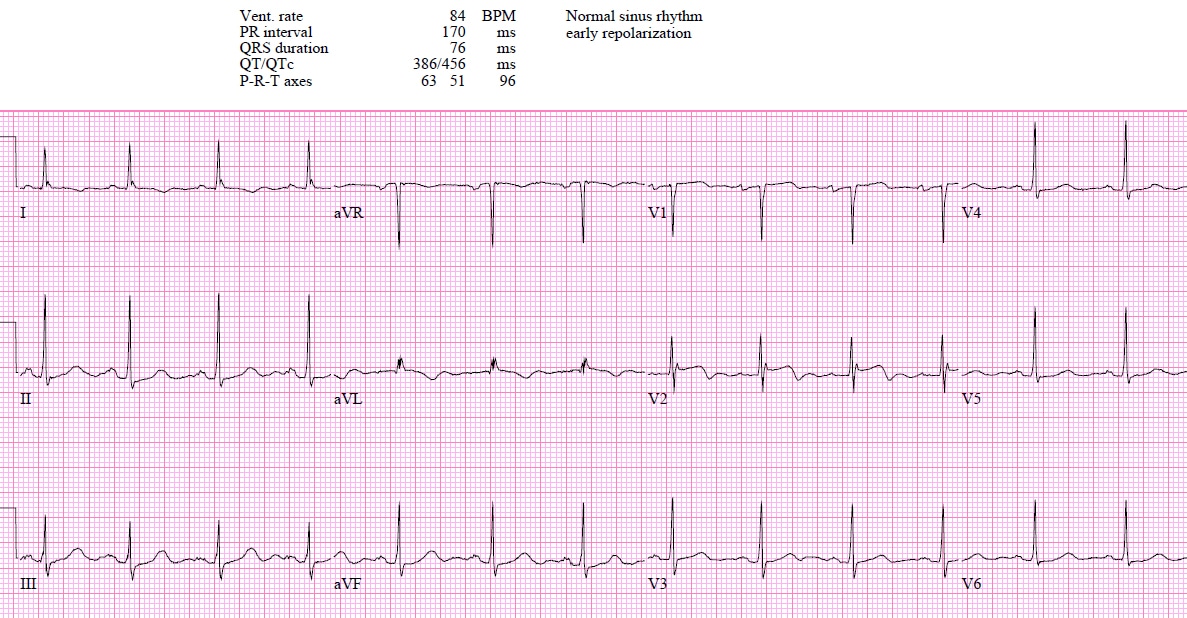
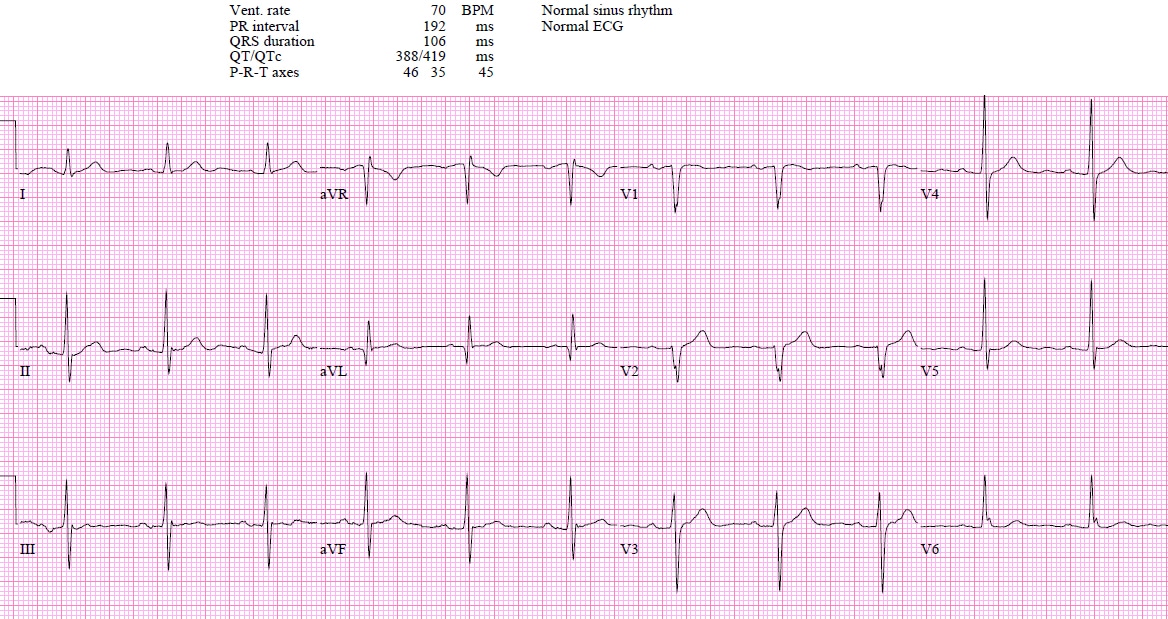
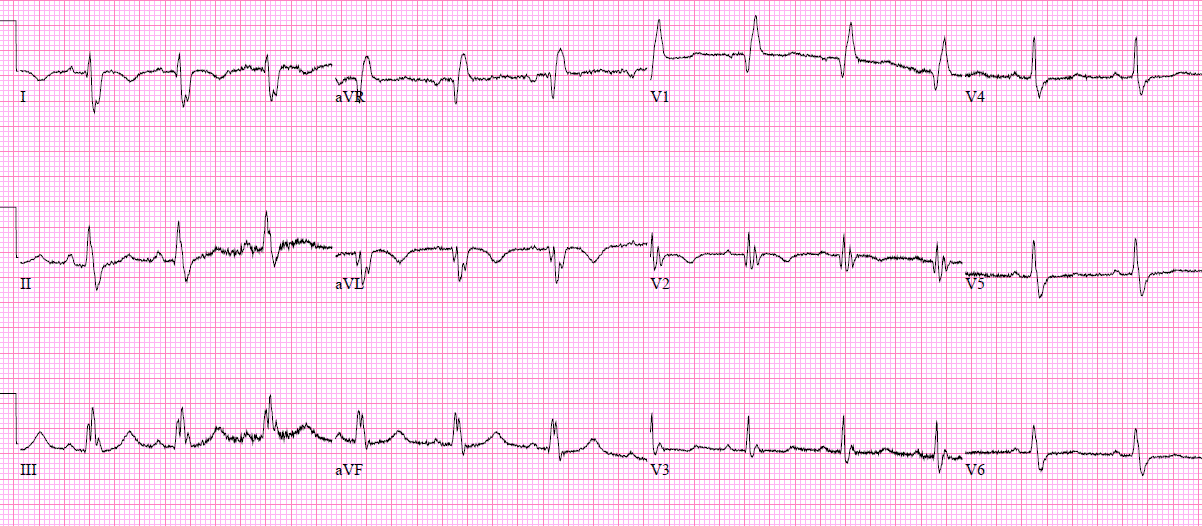
Patient 2: 60yo with epigastric pain, shortness of breath and sweating
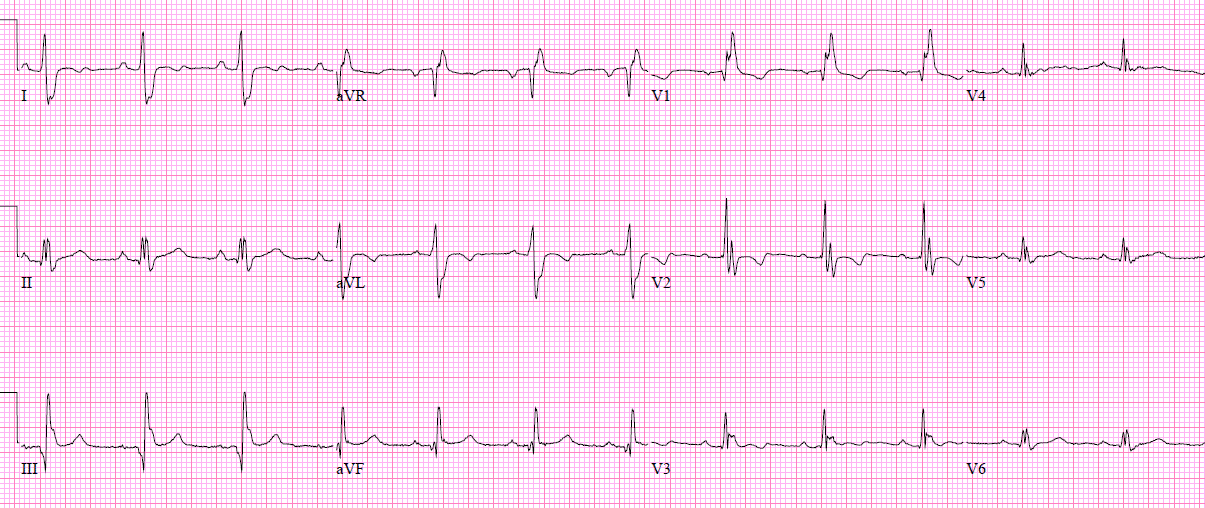
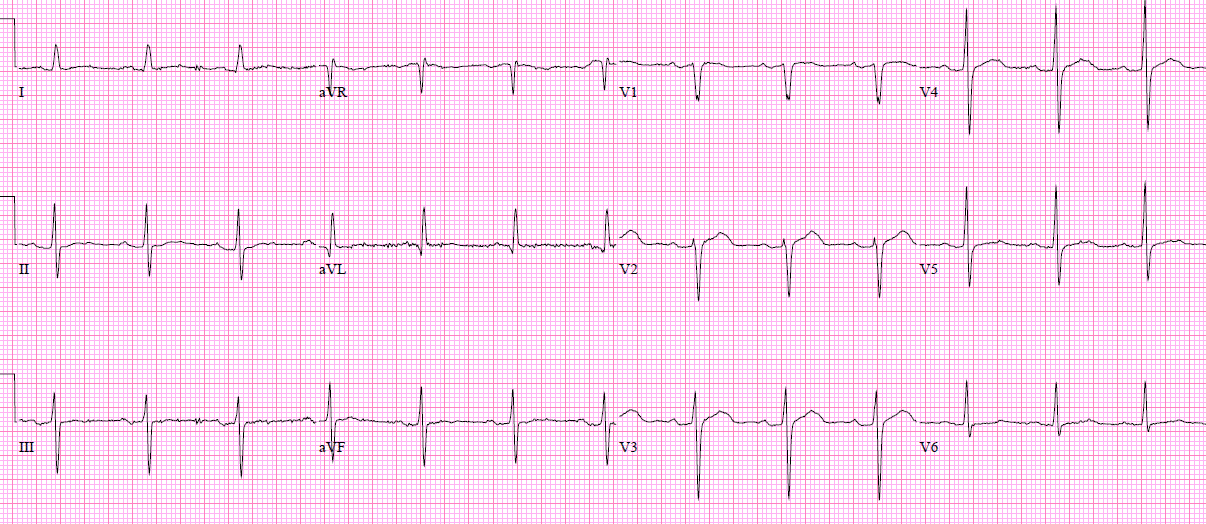
Patient 3: 65yo with 90 minutes of severe chest pain and hypertension
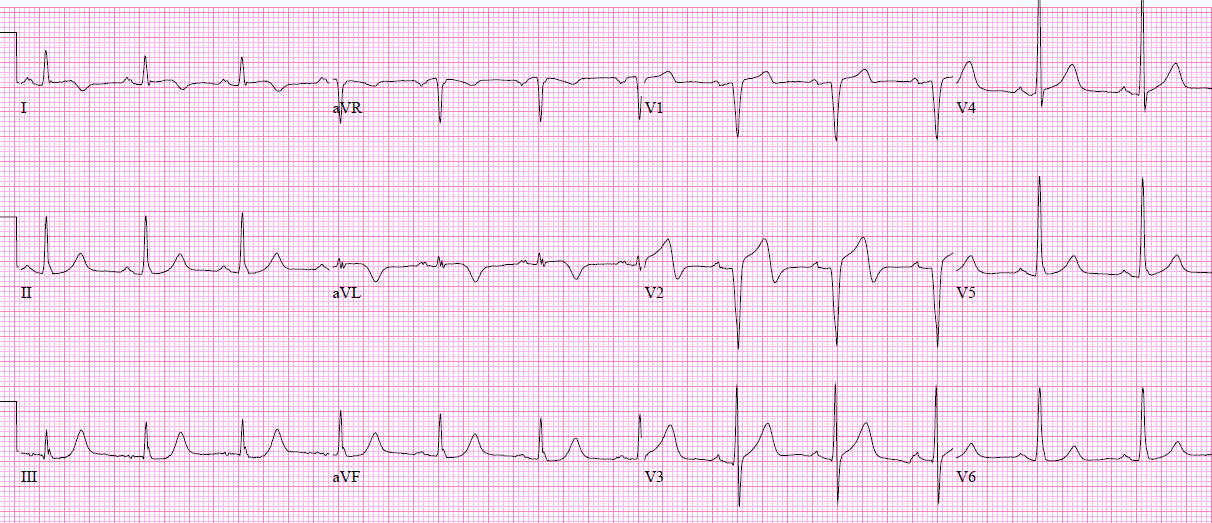
Patient 4: 60yo with 1 hour chest pain to the jaw, resolving but still present. Old then new ECG
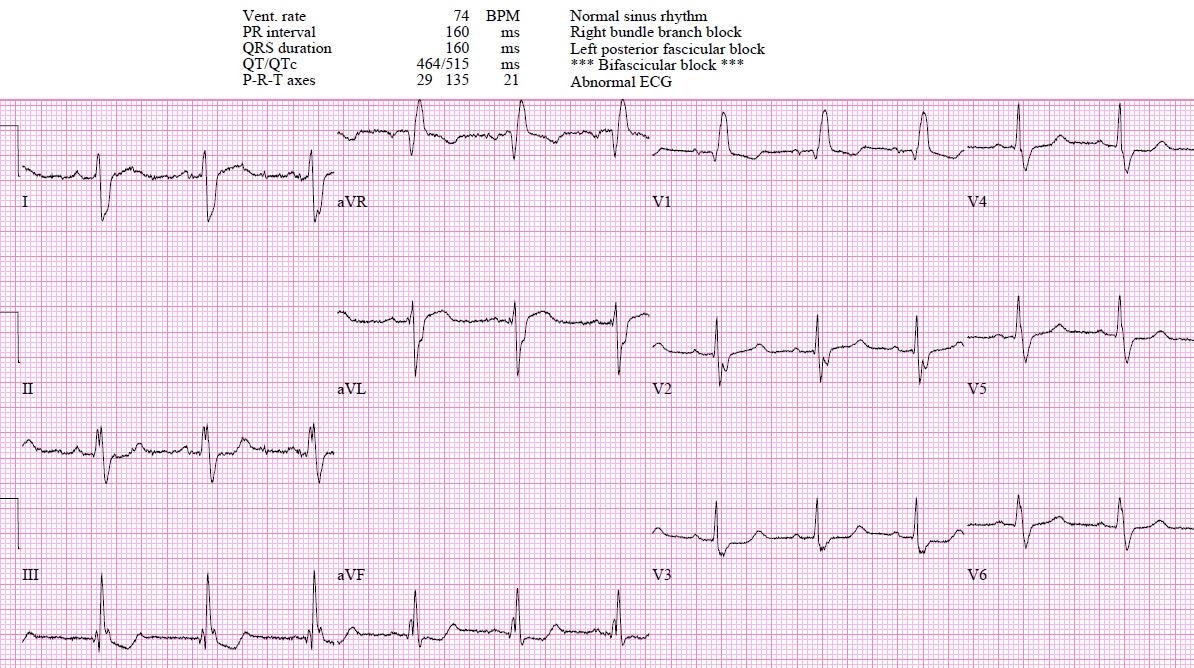
Patient 5: 45yo CABG to LAD/diagonal/RCA with 2 hours of chest pain. Old then new ECG:
Patient 6: 75yo prior RCA stent with 2 weeks exertional chest pain resolves with rest. Pain free and trop negative. Old then new ECG
First diagonal occlusion
STEMI is defined as ST elevation in two contiguous leads of at least 1mm (and greater in V2-3 based on age/sex), in the absence of LVH or LBBB. However, an occlusion of the first diagonal branch of the left anterior descending artery (LAD), which runs diagonally over the left ventricle to supply its anterolateral wall, often defies this classification. The resulting missed MIs are often associated with poorer outcomes. Although they are traditionally considered noncontiguous leads, ST elevations in aVL and V2 (with concurrent inferior ST depressions) should prompt a consideration of diagonal branch occlusion.[1]
This pattern was recognized 25 years ago, and differentiated from other occlusions that can cause ST elevation in aVL: “ST-segment elevation in lead aVL during AMI indicates either proximal LAD artery, Diagonal, or Obtuse Marginal [branch of circumflex] occlusion. If ST-segment elevation is found in aVL and the precordial leads V2 through V5, the culprit lesion is most probably located in the proximal portion of the LAD artery before the origin of the first diagonal branch. ST-segment elevation in leads aVL and V2, accompanied by either isoelectric or depressed ST segment in leads V3 through V6, favors occlusion of the first diagonal branch. ST elevation in aVL accompanied by isoelectric or negative ST segment in the precordial leads, including V2, predicts obstruction of the first obtuse marginal branch.” [2]
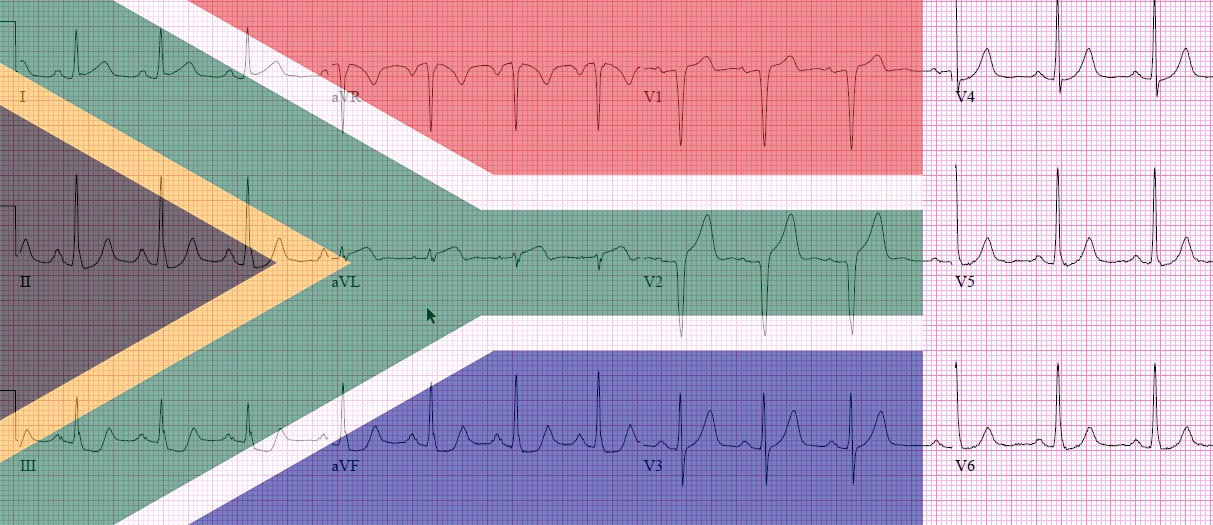
When first diagonal branch occlusion causes ST elevation in I, aVL and V2 along with inferior ST depression, it has been called the “South African flag sign“: The distribution of ST-segment deviation resembles the pattern of the South African flag with ST elevation in the upper left panel (lead I) and in the two middle panels in the second and third columns (leads aVL and V2, respectively), and ST depression in the bottom left panel (lead III). [3] Learning this classic pattern can help identify more subtle cases of first diagonal occlusion (or occasionally LAD occlusion, depending on coronary anatomy). While ST elevation in I and aVL will potentially meet classic STEMI criteria, diagonal occlusion will often not meet STEMI criteria–because the ST elevation involves noncontiguous leads aVL and V2, and/or because the degree of elevation is subtle and other signs of occlusion are needed to make the diagnosis (like new Q waves, pseudonormalized or hyperacute T waves, reperfusion T wave inversion, or reciprocal changes). First diagonal occlusion therefore serves as another reason for a paradigm shift from ST elevation MI (STEMI) to Occlusion MI (OMI).
Back to the cases
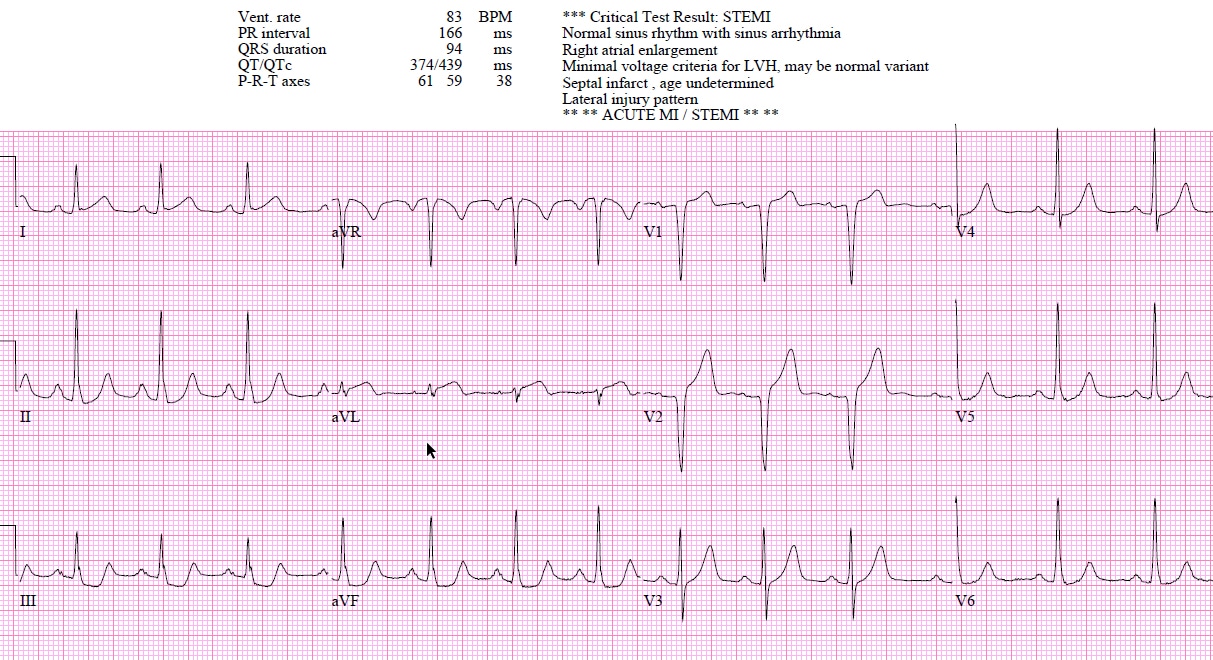
Patient 1: borderline STEMI(+), clear OMI(+) from diagonal occlusion
- Heart rate/rhythm: NSR
- Electrical conduction: normal intervals
- Axis: normal
- R-wave height/transition: normal except for Q wave in V1-V2
- Tension: LVH
- ST/T waves: borderline ST elevation V1-2, in the context of LVH. But there are hyperacute T waves in aVL/V2 and straightening of ST in I, along with inferior ST depression
Not clear STEMI but physician was concerned about aVL/V2 so stat cardiology consult. Cath lab activated: first diagonal occlusion. Discharge ECG had reperfusion T wave inversion in I, aVL and V2
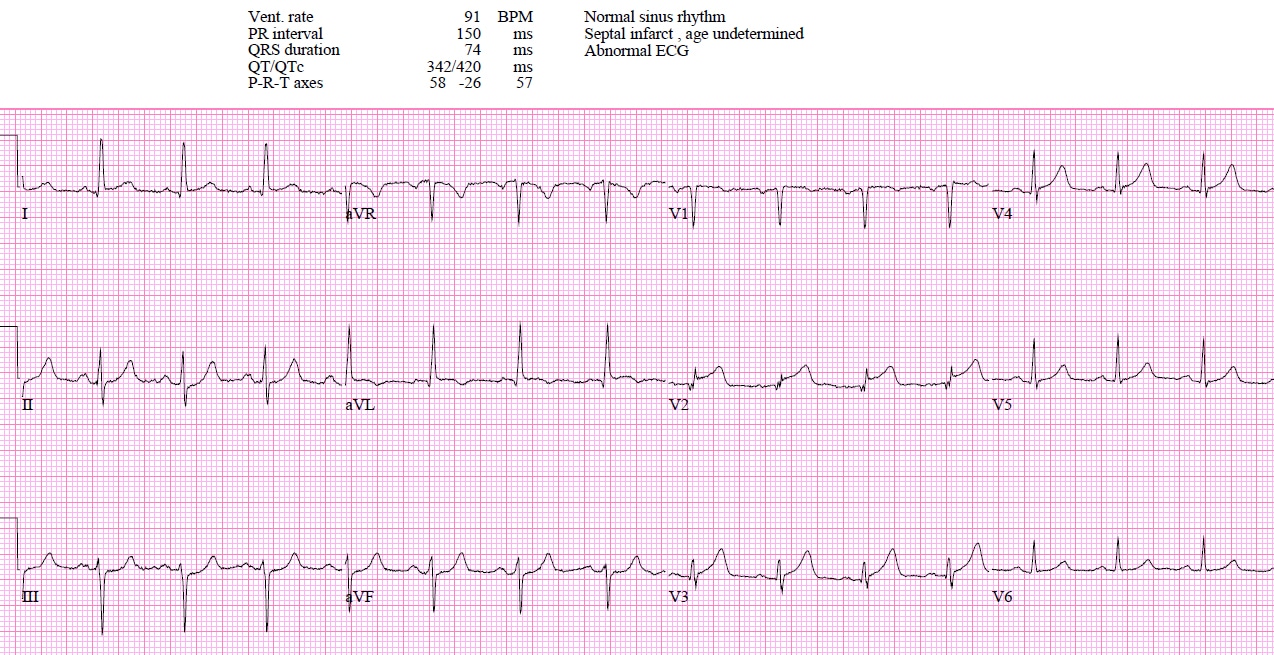
Patient 2: STEMI(-), OMI(+) from diagonal occlusion
- Heart rate/rhythm: NSR
- Electrical conduction: normal intervals
- Axis: left
- R-wave height/transition: normal except small Q in V2
- Tension: no hypertrophy
- ST/T waves: ST elevation and terminal QRS distortion in V2 (no S wave or J wave), subtle ST elevation aVL, and inferior ST depression
No STEMI criteria but physician was concerned about V2 so stat cardiology consult. Cath lab activated: diagonal occlusion. Discharge ECG had Q waves and reperfusion T wave inversion in I, AVL and V2:
Patient 3: STEMI(-), OMI(+) from diagonal SCAD
- Heart rate/rhythm: NSR
- Electrical conduction: normal intervals
- Axis: normal
- R-wave height/transition: normal
- Tension: no hypertrophy
- ST/T waves: V2 has fragmented QRS, terminal QRS distortion and hyperacute T wave (way bigger than entire QRS complex), and there’s non-concave ST elevation in aVL, with inferior ST depression
Another ischemic ECG called “normal” by the computer. Code STEMI activated. Because of severe chest pain and hypertension a CT was first done to rule out aortic dissection, and when that was negative patient was taken for cath: Spontaneous Coronary Artery Dissection (SCAD) of the first diagonal. Treated medically.
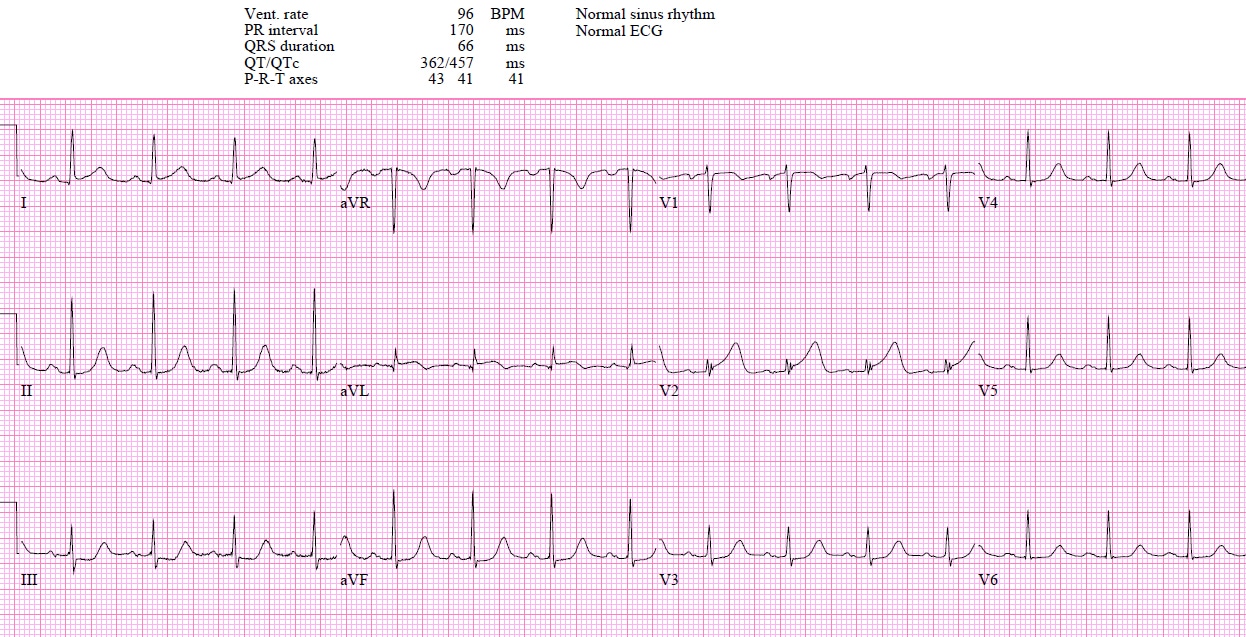
Patient 4: STEMI(-), OMI(+) reperfusing from LAD occlusion mimicking diagonal occlusion
- Heart rate/rhythm: NSR
- Electrical conduction: normal intervals
- Axis: normal
- R-wave height/transition: normal
- Tension: no hypertrophy
- ST/T waves: no change in ST segment amplitude but there is T wave inversion in V2 (and I/aVL) and inferior ST depression, which are exclusion criteria for early repolarization
No STEMI criteria so referred as NSTEMI when trop came back at 400, but mimics spontaneously reperfusion diagonal OMI (with resolving symptoms and T wave inversion in I/aVL/V2). Cath lab activated: 95% LAD occlusion with 50% diagonal ostial stenosis, peak trop 3000. Discharge ECG: anterolateral T wave inversion as expected for LAD occlusion
Patient 5: STEMI(-), OMI(+) from CABG diagonal graft occlusion
- Heart rate/rhythm: NSR
- Electrical conduction: old RBBB and LPFB
- Axis: old RAD from LPFB
- R-wave height/transition: tall R wave from RBBB
- Tension: no hypertrophy
- ST/T waves: mild relative ST elevation I/aVL/V2 with pseudonormalized T waves, along with inferior ST depression
Cath lab activated: occluded CABG graft to the first diagonal. Discharge ECG return of T wave inversions:
Patient 6: unstable angina with small diagonal occlusion
- Heart rate/rhythm: NSR
- Electrical conduction: normal conduction
- Axis: normal
- R-wave height/transition: normal except for Q in V2
- Tension: no hypertrophy
- ST/T waves: no ST/T changes but there are new Q wave in aVL/V2
Patient with “normal” ECG and negative troponin could have been sent home but because of the new Q waves was referred for admission. Cath: occluded tiny first diagonal which was recanalized (but too small to stent), and 80% RCA stent occlusion which was re-stented. Discharge ECG had resolution of diagonal Q waves:
Take home points on first diagonal occlusion
- The “South African flag sign” teaches the classic findings of first diagonal occlusion: ST elevation in I, aVL and V2 with inferior reciprocal changes
- In many cases first diagonal occlusion won’t meet STEMI criteria, but OMI can be identified by ST elevation in noncontiguous leads aVL/V2, other signs of occlusion in those leads (new Q waves, non-concave ST segments, hyperacute or pseudonormal T waves, reperfusion T wave inversion) along with inferior reciprocal changes.
References for ECG cases 8: first diagonal occlusion
- Durant E, Singh A. Acute first diagonal artery occlusion: a characteristic pattern of ST elevation in noncontiguous leads. Am J Emerg Med. 2015;33(9):1326.e3-5.
- Birnbaum Y, Hasdai D, Sclarovsky S, et al. Acute myocardial infarction entailing ST-segment elevation in lead aVL: electrocardiographic differentiation among occlusion of the left anterior descending, first diagonal, and first obtuse marginal coronary arteries. Am Heart J. 1996;131(1):38-42.
- Littmann L. South African flag sign: a teaching tool for easier ECG recognition of high lateral infarct. Am J Emerg Med. 2016;34(1):107-9.





The article was very helpful. I work EMS and this will help me look for a lateral occlusion.
what is the current evidance for thrombolysis for D1 occlution ?
I’m not aware of any studies that have looked at this question specifically. But as one review summarized: “STE in leads aVL and V2 can be the sole STE manifestations of a high-risk ECG presentation; such presentations can involve large amounts of myocardium in jeopardy situated in the anterior wall region of the left ventricle. Recognition and altered management of these lesions in a more aggressive fashion can be indicated in certain situations.” (Macias et al. The electrocardiogram in the ACS patient: high-risk electrocardiographic presentations lacking anatomically orienited ST-segment elevation. AJEM 34(2016): 611-617)