Topics in this EM Quick Hits podcast
Brit Long on Surviving Sepsis Campaign: 2021 Updates (0:38)
Nour Khatib on rural medicine case: angle closure glaucoma (11:59)
Reuben Strayer on bougie vs endotracheal tube and stylet on first-attempt intubation (20:51)
Justin Hensley on management of frostbite (31:35)
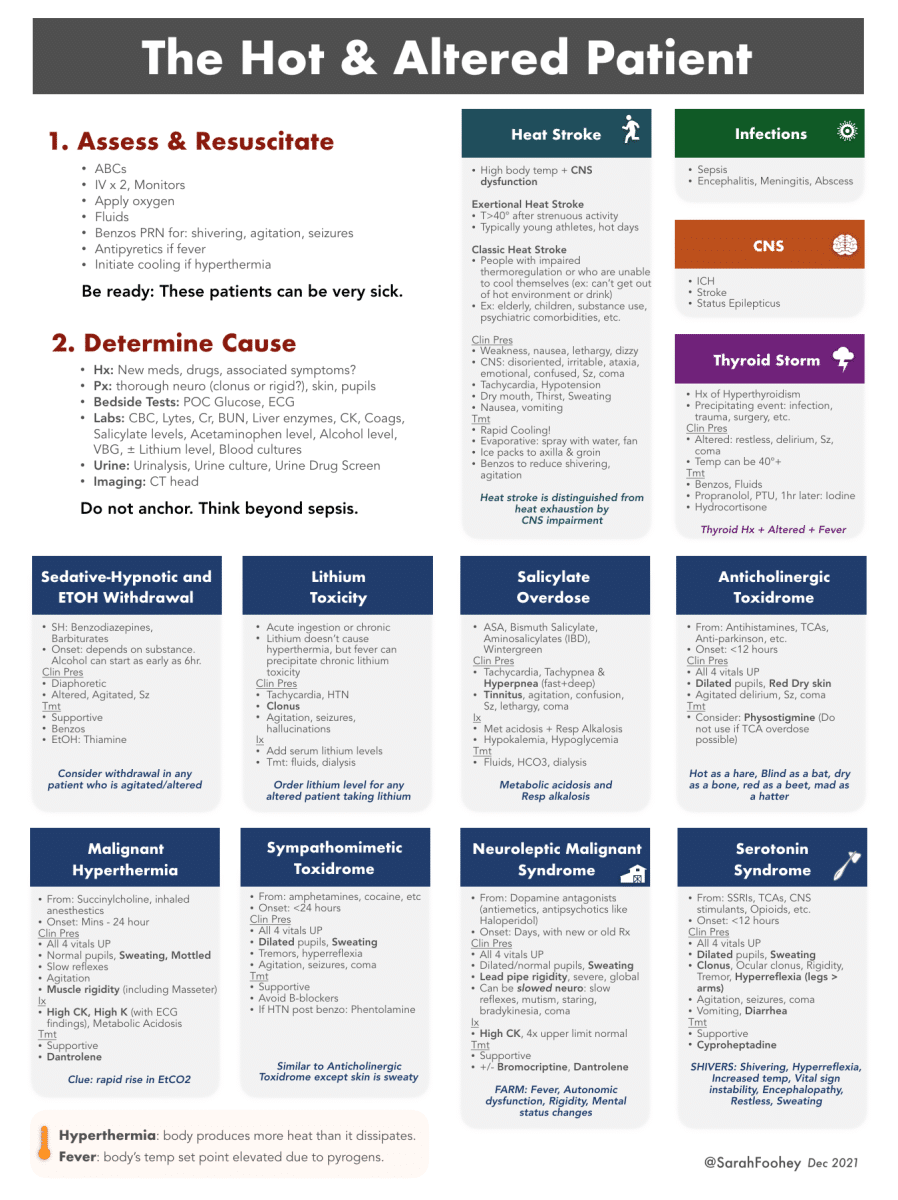
Sarah Foohey on the hot and altered patient (39:50)
Andrew Petrosoniak on central cord syndrome (47:47)
Podcast production, editing and sound design by Anton Helman
Podcast content, written summary & blog post by Raymond Cho, edited by Anton Helman
Cite this podcast as: Helman, A. Long, B. Khatib, N. Strayer, R. Hensley, J. Foohey, S. Petrosoniak, A. EM Quick Hits 36 – Surviving Sepsis, Angle Closure Glaucoma, Bougies, Frostbite, Hot/Altered Patient, Central Cord Syndrome. Emergency Medicine Cases. March 2022. https://emergencymedicinecases.com/em-quick-hits-march-2022/. Accessed [date].
Surviving Sepsis Campaign: 2021 Updates relevant to EM
Screening for Sepsis
- New guidelines recommend against using qSOFA as a single screening agent
- Commentary: NEWS score is likely a better single screening tool that is easy to use and can be done at triage
Resuscitation
- Fluids
- Guidelines now only suggest rather than recommend using 30 cc/kg of IV crystalloid within the first 30 minutes of resuscitation
- Balanced crystalloids such as Plasmalyte and Lactated Ringer’s recommended as a first line over normal saline
- Vasopressors
- In most patients, norepinephrine is the first-line vasopressor, followed by vasopressin, then epinephrine
- In patients with cardiac dysfunction, use norepinephrine as first line then dobutamine or epinephrine alone
- In septic shock resistant to vasopressors, guidelines now support using IV hydrocortisone
- Monitoring resuscitation
- Use dynamic parameters (e.g. passive leg raise, stroke volume/pulse pressure variation, ultrasound) rather than using static parameters
- Point-of-care ultrasound can be used to assess volume status (IVC, B-lines, cardiac activity)
- For patients in septic shock, target a MAP of 65 mmHg
- Adjunctive markers: use capillary refill, lactate to guide resuscitation
- Antimicrobial therapy
- In patients with possible sepsis without shock, consider investigating for other causes for up to 3 hours before starting antimicrobial therapy (adjusted from 1 hour from previous guidelines)
- Choice of antimicrobials in the empiric phase
- High risk of multi-drug resistant organisms: 2 agents with gram negative coverage
- Low risk of multi-drug resistant organisms: 1 agent with gram negative coverage
- High risk of MRSA: provide coverage for MRSA (eg. vancomycin)
- No risk factors for MRSA: no routine MRSA coverage
- Other
- IV vitamin C is not recommended in septic shock
Update 2023: A multicenter randomized controlled trial including 1563 patients with sepsis-induced hypotension refractory to initial treatment with 1-3L of IV fluids comparing a restrictive fluid strategy (prioritizing vasopressors and low intravenous fluid volumes) and a liberal fluid strategy (prioritizing higher volumes of intravenous fluid before vasopressor use) found that death from any cause before discharge home by day 90 was not significantly different between the two groups (14.0% vs 14.9% respectively, estimated difference -0.9%, 95% CI -4.4 to 2.6, P=0.61) (CLOVERS trial). Abstract
Airway and ventilation
- High-flow nasal cannula (HFNC): in sepsis-induced hypoxemic respiratory failure, HFNC is recommended over non-invasive positive pressure ventilation
- Intubation: low tidal volume strategy and upper plateau pressure of 30 cm H2O; in ARDS, consider using higher PEEP
- V-V ECMO can be considered if conventional mechanical ventilation fails
Episode 122 Sepsis and Septic Shock – What Matters from EM Cases Course with Sara Gray
- Evans L, Rhodes A, Alhazzani W, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock 2021. Crit Care Med. 2021 Nov 1;49(11):e1063-e1143.
- Evans L, Rhodes A, Alhazzani W, et al. Executive Summary: Surviving Sepsis Campaign: International Guidelines for the Management of Sepsis and Septic Shock 2021. Crit Care Med. 2021 Nov 1;49(11):1974-1982.
Rural Medicine Case: Angle Closure Glaucoma
Background
- Raised intra-ocular pressure due to impaired aqueous humour flow from posterior chamber
- This pushes the iris forward, closing the angle between the iris and the cornea
Clinical Presentation and Diagnosis
- Risk factors: medications that dilate the pupil (anticholinergics, TCAs, antiparkinsonian drugs, etc.), family history of glaucoma, hyperopic eyes, recent eye surgery
- Diagnosis: at least 2 of following symptoms – acute onset ocular pain with nausea and vomiting, intermittent blurring of vision with halo around lights, photophobia, vision loss
- Plus: at least 3 of following signs – intraocular pressure > 21 (typically >40), conjunctival injection, corneal epithelial edema, fixed mid-dilated pupil, shallow anterior chamber on slit lamp exam
Management and medications to consider
- Consult ophthalmology (definitive management is laser iridotomy)
- Pilocarpine 1-2 drops q15min for 2 doses (miotic)
- Timolol 0.25-0.5% 1 drop (beta blocker)
- Apraclonidine drops (alpha adrenergic agonist)
- Acetazolamide 500 mg IV x 1
- Mannitol 20% 1.25-2 g/kg IV x 1
- Reassess IOP q15min in the early phases
- Tintinalli J E, Cline D, Ma O John, et al. Tintinalli’s Emergency Medicine Manual 7/E. McGraw Hill Professional; 2012.
- Cargnelli S, Krywenky, A. Acute angle closure glaucoma review. (2016, October 8). CanadiEM. https://canadiem.org/medical-concepts-acute-angle-closure-glaucoma/
Bougie vs. Endotracheal Tube and Stylet on First-Attempt Intubation
Papers:
Driver et. al. (2018). Effect of use of a bougie vs endotracheal tube and stylet on first-attempt intubation success among patients with difficult airways undergoing emergency intubation. JAMA. Single-centre emergency department trial (BEAM Trial) at Hennepin County Medical Center.
Driver et. al. (2021). Effect of use of a bougie vs endotracheal tube with stylet on successful intubation on the first attempt among critically ill patients undergoing tracheal intubation. JAMA. Multi-centre trial at 7 emergency departments and 8 ICUs (BOUGIE Trial).
Clinical Question: does use of a tracheal tube introducer (“bougie”) increase the incidence of successful intubation on the first attempt, compared with use of an endotracheal tube with stylet?
Primary outcome: first-attempt intubation success in patients with at least one difficult airway characteristic
Results
- BEAM Trial (n = 757): first-attempt intubation success in patients was higher in the bougie group (98%) than in the endotracheal tube and stylet group (87%) (95% CI, 8-20%)
- BOUGIE Trial (n = 1102): there was no significant difference in first-attempt intubation success between the bougie group (80.4%) and the stylet group (83.0%) (95% CI, -7.3 to 2.2%, P = 0.27)
- Commentary: when the operator is experienced at using the bougie with a standard-geometry blade (i.e. emergency physicians at Hennepin County Medical Center), first-pass intubation success is very high. If the operator does not routinely use bougies, they do not confer a first-pass intubation success advantage
Advantages of bougie
- Better view of bougie passing through the cords; therefore, less likely to place the ETT in the esophagus
- Alternative ways to assess placement before placing ETCO2 monitor: feeling tracheal rings and being held up at the carina when advancing the bougie
Disadvantages of bougie
- Poor success with Grade 4 view (rare); when confronted with Grade 4 view consider alternative techniques

Respiratory Care, June 2014 Vol 59 No 6
Bottom Line: the bougie confers higher first-attempt intubation only when the operator is experienced using it. Use it regularly rather than only as a rescue device.
George Kovacs’ talk “What You Don’t Know About Bougies” from EM Cases Summit 2021 FOAMed
- Driver, B. E., Prekker, M. E., Klein, L. R., Reardon, R. F., Miner, J. R., Fagerstrom, E. T., Cleghorn, M. R., McGill, J. W., & Cole, J. B. (2018). Effect of use of a bougie vs endotracheal tube and stylet on first-attempt intubation success among patients with difficult airways undergoing emergency intubation. JAMA, 319(21), 2179.
- Driver, B. E., Semler, M. W., Self, W. H., Ginde, A. A., Trent, S. A., Gandotra, S., Smith, L. M., Page, D. B., Vonderhaar, D. J., West, J. R., Joffe, A. M., Mitchell, S. H., Doerschug, K. C., Hughes, C. G., High, K., Landsperger, J. S., Jackson, K. E., Howell, M. P., & Robison, S. W. (2021). Effect of use of a bougie vs endotracheal tube with stylet on successful intubation on the first attempt among critically ill patients undergoing tracheal intubation. JAMA, 326(24), 2488.
Management of Frostbite
First, manage hypothermia: rapid rewarming is most important
- Rewarm patient to a core temperature of 35°C before treating frostbite
- Remove all wet or constrictive clothing
CritCases 12 Accidental Hypothermia
Local Thawing
- Extremities: place in water with temp 37-39°C for 20-30 minutes
- Face: apply moistened compresses soaked in warm water
- Do not rewarm if there is any chance of refreezing
- Analgesia: be mindful that rewarming is very painful, so consider parenteral analgesia
- Local wound care: topical aloe vera cream, consider draining nonhemorrhagic bullae (in consultation with surgery), but leave hemorrhagic bullae alone; avoid antibacterial ointments
- Compartment syndrome: maintain high suspicion
Systemic Care
- In all patients
- Ibuprofen 12 mg/kg BID (2.4 g/d max)
- Tetanus prophylaxis
- If you think there is a chance of deep injury, consider using tPA and/or iloprost
- 3rd degree or higher: IV iloprost 2 ng/kg per min infusion, 6 h/d, for 5 days
- 4th degree: tPA 3 mg IV bolus then 1 mg/hr and heparin within 12 hours of rewarming
Update 2022: A systematic review from 2019 including a total of 208 patients treated for frostbite with tPA found that all quality of evidence and data for thrombolysis in frostbite to be low. Abstract
Iloprost protocol for frostbite
Quick Hit 27 on iloprost for frostbite
- Hallam, M., Cubison, T., Dheansa, B., & Imray, C. (2010). Managing frostbite. BMJ, 341(nov19 1), c5864-c5864. https://doi.org/10.1136/bmj.c5864
- Handford, C., Buxton, P., Russell, K., Imray, C. E., McIntosh, S. E., Freer, L., Cochran, A., & Imray, C. H. (2014). Frostbite: A practical approach to hospital management. Extreme Physiology & Medicine, 3(1). https://doi.org/10.1186/2046-7648-3-7
- Poole, A., & Gauthier, J. (2016). Treatment of severe frostbite with iloprost in Northern Canada. Canadian Medical Association Journal, 188(17-18), 1255-1258. https://doi.org/10.1503/cmaj.151252
The Hot and Altered Patient
- Foohey, S. (2021, December 1). The Hot and Altered Patient. First10EM. https://first10em.com/fooheysfigures-diagnostic-approaches/
Central Cord Syndrome: Hyperextension injury of the c-spine with upper extremity weakness and a benign CT c-spine that is easy to miss
- This is an incomplete spinal cord syndrome (meaning there is some sensory and/or motor function below the level of the injury that may be only in the saddle/sacral region) so check these on physical examination
- It is a clinical diagnosis with upper extremity weakness (typically weakness in hands>arm>shoulder) greater than lower extremity weakness (findings may be subtle so a careful assessment of power is essential); in a minority of cases, there is some bowel/bladder dysfunction.
- The 3 predominant phenotypes are
- Elderly patients who have a low energy fall sustaining a hyperextension mechanism,
- High energy trauma (often MVC) that causes hyperextension in a younger patient or
- Patients with a fracture/dislocation of the c-spine
- CT is the test of choice in the ED and a CT-angiogram of the carotids should be considered as well; CT typically shows no fracture/dislocation and only degenerative disc disease; it is important to maintain a high index of suspicion regardless of the CT findings, even if the CT is normal; typically full spine MRI is done as an inpatient
- Ameer et al. Central Cord Syndrome. Dec 29, 2021. https://www.ncbi.nlm.nih.gov/books/NBK441932/
- Badhiwala et al. The case for revisiting central cord syndrome. Spinal Cord, 2020. 58:125-127. https://www.nature.com/articles/s41393-019-0354-5
- Nowak et al. Central Cord Syndrome. J Am Acad Orthop Surg 2009; 17:756-765.
None of the authors have any conflicts of interest to declare





Leave A Comment