In this episode, Dr. Jordan Chenkin & Dr. Jamie Blicker discuss positioning, landmarking, and best technique for lumbar puncture, how to minimize post-LP headache and traumatic taps, as well as when CT head is not required prior to LP. They discuss the indications, contraindications, trouble-shooting and pros and cons of needle aspiration, small bore pleural catheter with Heimlich valve and large bore chest tube for the treatment of spontaneous pneumothorax. Dr. Chenkin presents an intriguing argument for why he uses ultrasound-guided fracture reduction routinely in the ED, and we end with a few tips and tricks using skin adhesive for some unorthodox indications.
Written summary and blog post by Claire Heslop, edited by Anton Helman March, 2013
Cite this podcast as: Chenkin, J, Blicker, J, Helman, A. LP, Spontaneous Pneumothorax and Ultrasound Guided Fracture Reduction. Emergency Medicine Cases. March, 2013. https://emergencymedicinecases.com/episode-31-lumbar-puncture-spontaneous-pneumothorax-ultraound-guided-fracture-reduction/. Accessed [date].
LUMBAR PUNCTURE
Indications for CT before LP?
Herniation after LP is extremely rare. Mass effect on CT does not predict herniation, and normal CT does not eliminate the risk. Obtaining a CT prior to the LP can delay diagnosis and risk negative culture from the LP tap. Always give antibiotics before CT especially if delay is anticipated. Our experts recommend selective use of CT. Clinical findings can be used to identify patients who need a CT scan and guidelines from the Infectious
Diseases Society of America identified six indications for CT head before LP:
- History of immune compromise
- Known focal CNS disease
- Seizure in the past week
- Papilledema
- Altered LOC
- Focal deficit on exam
Ultrasound can be used to assess optic nerve diameter for papilledema. The basic technique involves applying a high frequency linear probe on the patient’s closed eyelid with a neutral gaze. Find the optic nerve in the retina surface, and measure optic nerve sheath diameter at a point 3 mm posterior to the retina. >5 mm diameter is abnormal, as is a convex bulge in the optic nerve, which suggests papilledema.
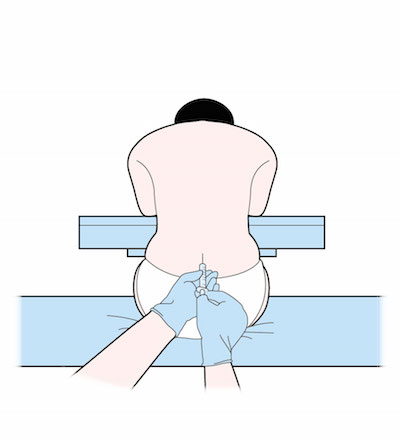
What’s the Best Position for LP?
There is no evidence that one position is best for the LP, but opening pressures are only accurate in lateral decubitus. This position may also help the patient stay still, and prevents a fall if syncope occurs. Remember to fully align the spine, with hips perpendicular to the bed, and a pillow under the head. If choosing a sitting position, which may optimize interspace diameter, place feet on a stool to flex hips, and don’t over flex the neck.
Tips for a “Champagne Tap”
- Our experts recommend using lidocaine with epinephrine to create a wide anesthesia field, and inserting the needle through sterile 2×2” gauze.
- Clean the head of the needle if blood appears at the initial part of the tap to avoid contaminating the entire sample with RBCs from the initial clot.
- Only reposition/re-angle the needle when it is withdrawn to the skin surface, and consider moving to another interspace rather than reattempting at the same site to reduce the risk of a traumatic tap.
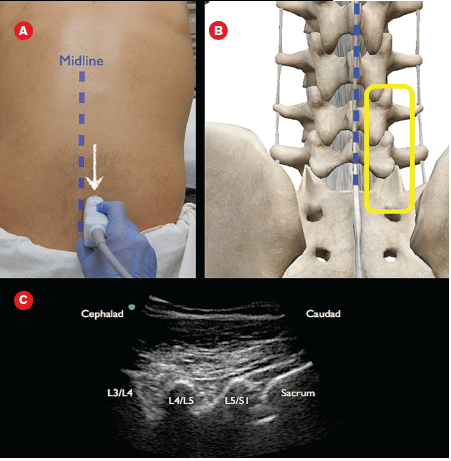
Ultrasound guided lumbar puncture
- Ultrasound can be used if landmarks are not palpable, to improve accuracy without adding to procedure time. Position the patient for the LP and use curved array probe in the transverse and mark the midline. Then estimate the distance required to reach the ligamentum flavum, and the angle required for the needle, and turn the probe to longitudinal to find and mark the interspace.
- For certain patients who cannot flex their back, a lateral (aka paramedian approach) may help.
- Insert the needle 1 cm lateral to the midline, and direct it slightly cephalad and medially to reach the midline.
Video on ultrasound guided lumbar puncture
SPONTANEOUS PNEUMOTHORAX
Asymptomatic patients without lung pathology who have a small (only observation and a repeat CXR. Spontaneous pneumothoraces that are larger or symptomatic, or secondary to lung pathology should be treated.
For primary pneumothorax, evidence suggests needle aspiration is noninferior to chest tube drainage. A 14 or 16G angiocath connected to a 3 way stopcock can be used for serial aspirations with a large syringe.
Pigtail catheters/small bore pleural catheters with a Heimlich valve may be used instead. They produce less pain than a chest tube, and allow for outpatient management, however they tend to kink, clog, and displace so require careful insertion and followup. An outpatient protocol using small bore pigtail catheters demonstrated >80% success rate for resolution and patient discharge home.
Tips for Pleural Catheter Insertion
- Do not tunnel the catheter on insertion (or it will kink) – insert the catheter straight in, over the rib to avoid the neuro-vasc bundle
- Angle the tube toward the apex and insert to the hub, then attach the Heimlich valve
- Warn the patient pleural fluid may drain, and they may loosely attach an open bag to catch the fluid
Pleural catheters are usually not suitable for secondary pneumothoraces, as these have a high rate of re-occurrence and risk of tension pneumothorax. Also, they should not be used if blood, pus, or large amounts of pleural fluid are present. These patients all need a large-bore chest tube, and admission to hospital. Our experts recommend if patients are discharged with pleural catheters, using a standard flow-sheet with assessments every 24 hours and a stepwise advancement of methods if it does not initially resolve. (I.e. low GOMCO suction if underwater seal alone does not work.)
HOW TO REDUCE A FRACTURE WITH ULTRASOUND
Ultrasound-guided fracture reduction in the ED
Cortical and cortex disruption shows up well on ultrasound, thus ultrasound can be used to visualize occult fractures (sternum, scaphoid, rib), to guide needle positioning for a hematoma block, and to verify success of fracture reduction.
Using ultrasound may improve success of fracture reduction.
Procedure for U/S imaging for fracture reduction:
- Position the limb for reduction
- Use copious gel to float the probe above the skin, along the longitudinal axis, and center over the cortex
- Side proximal/distal to visualize the fracture and assess angulation
- Save the image on the machine
- Perform the reduction and recheck the fracture appearance (before splinting) to verify success.
Ultrasound guided distal radius fracture reduction on Ultrasound Podcast
Dr. Helman, Dr. Chenkin and Dr. Blicker have no conflicts of interest to declare.
For more on pneumothorax on EM Cases:
Journal Jam 2: Small Bore Chest Tube and Outpatient Management of Pneumothorax
POCUS Cases 2 Pneumothorax
References
Alcock, A., and R. Salter. “Towards evidence-based emergency medicine: best BETs from the Manchester Royal Infirmary. BET 2: what gauge and type of lumbar puncture needle should we be using in the paediatric population to reduce the risk of postdural puncture headaches?.” Emergency medicine journal: EMJ 30.1 (2013): 80-81. www.ncbi.nlm.nih.gov/pubmed/?term=Alcock+A%2C+Sa…
Hasbun, Rodrigo, et al. “Computed tomography of the head before lumbar puncture in adults with suspected meningitis.” New England Journal of Medicine 345.24 (2001): 1727-1733. www.ncbi.nlm.nih.gov/pubmed/?term=Hasbun+R+et+al…
Nomura, Jason T., et al. “A randomized controlled trial of ultrasound-assisted lumbar puncture.” Journal of Ultrasound in Medicine 26.10 (2007): 1341-1348. www.ncbi.nlm.nih.gov/pubmed/?term=Nomera+JT+et+a…
Tunkel, Allan R., et al. “Practice guidelines for the management of bacterial meningitis.” Clinical infectious diseases 39.9 (2004): 1267-1284. www.ncbi.nlm.nih.gov/pubmed/?term=Tunkel+AR+et+a…
Hassani, Behzad, John Foote, and Bjug Borgundvaag. “Outpatient Management of Primary Spontaneous Pneumothorax in the Emergency Department of a Community Hospital Using a Small‐bore Catheter and a Heimlich Valve.” Academic Emergency Medicine 16.6 (2009): 513-518. www.ncbi.nlm.nih.gov/pubmed/?term=Hassani+B+et+a…
Zehtabchi, Shahriar, and Claritza L. Rios. “Management of emergency department patients with primary spontaneous pneumothorax: needle aspiration or tube thoracostomy?.” Annals of emergency medicine 51.1 (2008): 91-100. www.ncbi.nlm.nih.gov/pubmed/?term=Zehtabchi+S%2C…
Ang, Shiang-Hu, Shu-Woan Lee, and Kai-Yet Lam. “Ultrasound-guided reduction of distal radius fractures.” The American journal of emergency medicine 28.9 (2010): 1002-1008. www.ncbi.nlm.nih.gov/pubmed/?term=Ang+SH+et+al.+…





Thanks a lot for the talks. I like the phish as well. I was wondering if next time you talk about LPs you could comment on how long people wait for equilibration to record opening pressure and relation to needle size (so if you are using one of the small 26g needles how long do you wait?). Also you could ask the guests about effect of positioning on pressure reads. Anyway thanks again.
Thanks for your great questions. The standard for opening pressure position is lateral decubitus. I prefer starting the LP sitting and then, with the LP needle in place, carefully converting them to lateral decubitus for the opening pressure. I do not know of any time differential related to needle size. Anyone else know? Anton