Whistler’s Update in Emergency Medicine Conference 2013 in Whistler, British Columbia is U of Toronto’s case-based interactive small group EM conference. There were so may great talks with amazing clinical pearls that I decided to wade through the 18 hours of audio recordings and packaged some of the key highlights for you here……EM Literature Review 2012 by Dr. Joel Yaphe, Neonatal Resuscitation Pearls by Dr. Nicole Kester-Greene, Fever of Unknown Origin by Dr. Shirley Lee, Improving Cosmesis in Wound Management by Dr. Maria Ivankovic, Hepato-biliary Disease by Dr. Sara Gray, & Pediatric Cardiac & Respiratory Cases by Dr. Donna Goldenberg.
Written summary and blog post by Claire Heslop, edited by Anton Helman April, 2013
Cite this podcast as: Yaphe, J, Lee, S, Ivankovic, M, Helman, A. Whistler Update in Emergency Medicine Conference 2013. Emergency Medicine Cases. April, 2013. https://emergencymedicinecases.com/episode-32-whistlers-update-in-emergency-medicine-conference-2013/. Accessed [date].
EM LITERATURE REVIEW 2012 from Whistler’s Update in Emergency Medicine Conference 2013
Head Bleeds and Anticoagulants
Ann Emerg Med (2012) 59:451–55.
- 16% of Warfarin patients with minor head injury had a bleed on the initial CT. After a negative CT, 6% had a delayed bleed on 24hr CT, and one patient required surgery.
Ann Emerg Med (2012) 59:460–8.
- In patients with head injuries, 5% of patients on Warfarin, and 12% of patients on clopidogrel had a bleed on initial CT. No clopidogrel patients had a delayed bleed in this study.
Dr. Yaphe concludes: we should strongly consider a head CT for clopidogrel patients with minor head injury, given the high bleeding rate observed. While patients on Warfarin may not need 24h observation, if you are worried about bleed risk for whatever reason, consider a repeat CT in 24hrs, with observation at home or in hospital.
Can Patients Remove their own Sutures?
CJEM (2012) 14:219–23.
- Given proper instructions and basic equipment, many patients are willing and able to remove their own sutures. (>90% success in intervention group)
Identifying and Treating Acute Bacterial Rhinosinusitis
Clin Infect Disease (2012) 54:e72–112.
- IDSA guideline recommendations for identifying acute bacterial vs. viral rhinosinusitis. Recommendations are to treat with antibiotics if 1. symptoms (purulent discharge and pain/tenderness on face or teeth) are present for >10d without improvement, or 2. if symptoms are severe or fever >39 + symptoms >3d, or 3. if symptoms occur at the end of a URTI that lasted 5-6 days that was initially improving (“double sickening”)
- 1st line treatment: Amox/Clav 500/125 tid or 875/125 bid for 5–7 days in adults, and 10–14 days in children.
- 2nd line treatment: Amox/Clav 2000/125 bid or Doxycycline 100 bid (or 200 od).
Ultrasound-Guided Management of Peritonsillar Abscess
Acad Emerg Med (2012)19:626–31.
- This prospective RCT suggested that diagnosic accuracy and aspiration success was greatly improved by using intracavitary ultrasound, and U/S use reduced ENT consults and CT use.
See Episode 38 on ENT Emergencies with Leeor Sommer and Maria Ivankovic for more on peritonsillar abscess drainage
Patient Controlled Analgesia (PCA) for Acute Abdominal Pain
Acad Emerg Med (2012)19(4):370-7
- Patients with abdominal pain
- More patients in the PCA arms reported satisfaction and did not require further analgesics at 2hrs compared to non-PCA patients. Although these were small doses and carefully-selected patients,
- PCA may have a role in the ED.
Azithromycin and Risk of Cardiovascular Death
Large retrospective study observed a small absolute increase in CV death with azithromycin versus other antibiotics, which was more pronounced in patients with a high baseline risk for CV disease.
Gonorrhea is Cefixime Resistant
JAMA. (2013) Jan 9;309(2):163-70
- Prospective study in Toronto testing gonorrhea cefixime sensitivity and cure rate. They showed 7% treatment failure with cefixime suggesting sufficient antibiotic resistance exists. Ceftriaxone (IV/IM) may be a better choice for treating uncomplicated gonorrhea.
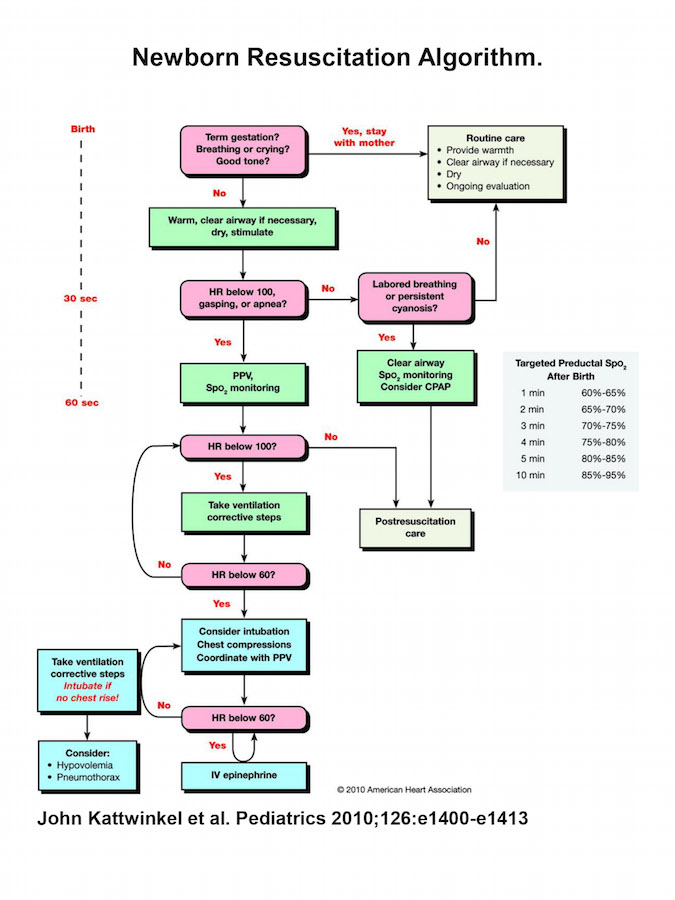
Neonatal Resuscitation Guidelines
Simplified Algorithm
- Avoid Hyperoxygenating
- Heart rate is most important assessment, (rather than colour), and preductal SaO2 should be used in assessment
- Resuscitate on room air rather than 100% oxygen
- Normal preductal SpO2 takes 10 minutes to reach 95% (see above)
- Routine intrapartum suctioning is not recommended – only suction if baby is not vigorous and meconium is present. In that case, suction prior to stimulating
- Delay cord clamping (>60 sec) in babies not requiring resuscitation
- Achieve adequate ventilation.Deliver gentle inflation pressures, ensure the mask and airway are well positioned, and use suction, positive pressure, or intubation if necessary before starting chest compressions
- Therapeutic hypothermia has a role for newborns with hypoxic ischemic encephalopathy
FEVER OF UNKNOWN ORIGIN
From Whislter’s Update in Emergency Medicine Conference 2013
Fever of Unknown Origin Definition:
- Recurrent fever ≥38.3, with symptoms ≥3 weeks, & no diagnosis.
4 main etiology categories:
-
- Infection (25–30%)
- Neoplasm (20%)
- Collagen vascular disease (20%)
- Misc (10–20%) i.e. DVT/PE
Most commonly missed causes are:
- endocarditis
- osteomyelitis
- secondary rheumatic fever and
- TB in immigrant populations
Minimal workup (Internal Medicine Literature): CBC, lytes, blood films, lactate, LFT/enzymes, urine, ANA, Rh factor, HIV, hepatitis, CMV, and a chest x-ray.
Consider a CT abdomen, which has been shown to have as high as a 20% yield for abscesses and tumors in FUO, leg doppler or TEE depending on the patient. Remember to look for temporal arteritis (GCA) in elderly patients.
IMPROVING COSMESIS IN WOUND MANAGEMENT
Retained foreign bodies: Glass is the most common foreign body retained in a wound. Get an Xray! 99% of retained glass is radioluscent if >2mm in size.
Glue vs. Sutures?
- Glue is 6 minutes faster than suturing, and has comparable cosmesis in the right wounds. It is an appropriate option for linear, lowtension and clean wounds away from moist areas or mucosa.
- To apply: after irrigation and hemostasis, apply 3-5 layers of glue, with 30 seconds between coats. Avoid getting glue between wound edges.
- Protect eye area with a petrolatum-based ointment border.
For more tips and tricks on tissue adhesive skin glue go to Michelle Lin’s Academic Life in EM Blog.
Absorbable Sutures: Available evidence suggests absorbable sutures may have comparable cosmesis to non-absorbable. Consider this option for kids, and patients with poor follow-up.
Indications to suture Tongue Lacerations: Always examine for other injuries & missing teeth. Indications to suture are:
- >1-2 cm laceration,
- Large flaps or gaps that trap food,
- Significant bleeding, and
- Anterior split tongues.
Use sedation for children, and consider an inferior alveolar block.
Tie suture knots 4–5x but tie loosely to allow for swelling. Use chromic gut or vicryl (not fast absorbing) in 1 or even 2 layers.
Laceration Cosmetic Pearls:
- Evert edges—enter the skin at 90’ and making suture depth > width, and consider a mattress suture
- Minimize trauma to tissue—be gentle with instruments and use minimal suture size and tension
- Relieve wound tension at edges—tension increases scarring, so undermine wound edges at dermal-adipose juncture, and use a layered closure if necessary
- Use a corner stitch to preserve flap blood supply
- Use edge excision for rough edges of jagged wounds
Post-Suture Care
Polysporin or antibiotic ointment for 2–3 days only, and use a petrolatum based ointment after this time. Protect the scar from sun (hat, sunscreen) to prevent hyperpigmentation for several months.
Aloe has not been proven to show any benefit, and vitamin E may worsen scars.
Delayed Primary Closure
- Highly contaminated, devitalized, or crush wounds, and immunodeficient patients may benefit from delayed primary closure, which is underutilized.
- Copiously irrigate, debride visiblydevitalized tissue, and remove as much dirt as possible.
- Start prophylactic antibiotics, ideally within 6h, and have the wound re-evaluated in 3–5 days (ideally in a plastics clinic), for potential delayed primary closure.
HEPATO-BILIARY DISEASE
Cholycystitis
Ultrasound Diagnosis: A positive sonographic Murphy sign has >95% PPV for cholecystitis. Gallbladder wall thickness >3mm, and pericholecystic fluid also suggest cholecystitis.
Antibiotics for Cholycystitis: Evidence from Cochrane review suggests patients with mild cholecystitis do not benefit from antibiotics.
Early vs Delayed Surgery: early cholycystectomy (within 24hrs of Dx) may reduce hospital length of stay and rate of conversion to open cholecystectomy compared to delayed surgery (weeks after Dx)
Cholangitis
- High mortality rate
- Needs expeditious abx and decompression by ERCP.
- Charcot’s triad (jaundice, fever, RUQ pain) is only present in 1/3 of patients.
- Normal CBD diameter is
Hepatic Encephalopathy (HE)
A diagnosis of exclusion in patient with altered mental status and a history of liver cirrhosis. Asterixis have poor specificity and sensitivity for the Dx of HE. Serum Ammonia also has poor sensitivity and specificity, has limited value in the ED and can be misleading.
Look for signs of raised ICP as many patients will have cerebral edema requiring mannitol. Treat severe cases aggressively with fluid, Abx, and lactulose 45cc q1h until patient has BM, then 30cc tid.
Spontaneous Bacterial Peritonitis (SBP)
- Suspect SBP in liver disease patients ascites and abdominal pain.
- Absolute contra-indications to paracentesis (acute abdomen, DIC, thrombolysis) and relative contraindications (local cellulitis, distended bowel, adhesions) must be considered.
- Treat for SBP if paracentesis fluid neutrophils >250k, or pH <7.34, and send for culture.
PEDIATRIC CARDIAC & RESPIRATORY CASES
History for chest pain: Chest pain in kids is usually MSK, so ask about trauma, sports activity etc. Ask about recent viral illness (myocarditis), sickle cell history (acute chest syndrome) and previous chest pain.
About Myocarditis: usually viral etiology. The prodrome includes fever, myalgia, and then chest pain and eventually CHF +/- arrhythmia. Trop will usually be elevated. CXR and ECG may be normal. Do an echo and consult cardiology.
What about chest pain in sickle cell patients?
Acute chest syndrome is a common cause of chest pain in sickle cell disease and the most common cause of death. Clinical picture of penumonia with infiltrate on CXR.
Infiltrates usually appear after 2-3 days, and CXR findings underestimate lung involvement.
Treat with pain meds, oxygen, Abx and transfusions as indicated.
**NSAIDs may worsen sickle crisis**
Secondary non-traumatic pneumothorax: In pediatrics is associated with parenchymal lung disruption, such as asthma, CF, connective tissue disease, malignancy, and FB aspiration. For pediatrics, there is no accepted criteria for who needs drainage, and many patients do well with observation alone, without drainage.
Intubating kids with severe asthma: When possible, intubation should be avoided. Tracheal intubation aggregates bronchospasm, induces laryngospasm, increases barotrauma, and drops BP.
Update 2022: A multicenter database of 276,832 pediatric procedural sedations found that the overall adjusted prevalence of laryngospasm was 3.3/1000 children with the biggest risk factors being concurrent URI (12.2/1000) and those undergoing airway procedures (9.6/1000). This review also found that combination regimens were associated with increased laryngospasm when compared to a single agent. Abstract
When to intubate?? intubate for impending respiratory arrest, profound hypoxemia unresponsive to therapy, or rapid deterioration of mental status and metabolic parameters. Once intubated, avoid rapid normalization of CO2. Instead, tolerate mild hypercapnea by using slower minute ventilation rates (to avoid air trapping, which decreases venous return).
For further pearls about intubating severe asthmatics, see EM Cases episode 8.
None of the speakers have any conflicts of interest to declare.
References
Allen, Vanessa G., et al. “Neisseria gonorrhoeae Treatment Failure and Susceptibility to Cefixime in Toronto, CanadaN gonorrhoeae and Susceptibility to Cefixime.” JAMA 309.2 (2013): 163-170. www.ncbi.nlm.nih.gov/pubmed/?term=JAMA.+(2013)+J…
Alsakha, A., and A. Guttman. “Traumatic intracranial hemorrhage in patients using warfarin or clopidogrel.” CJEM 15 (2012): 1-3. www.ncbi.nlm.nih.gov/pubmed/?term=Ann+Emerg+Med+…
Birnbaum, Adrienne, et al. “Efficacy of Patient‐controlled Analgesia for Patients With Acute Abdominal Pain in the Emergency Department: A Randomized Trial.” Academic Emergency Medicine 19.4 (2012): 370-377. www.ncbi.nlm.nih.gov/pubmed/?term=Acad+Emerg+Med…
Chow, Anthony W., et al. “IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults.” Clinical Infectious Diseases 54.8 (2012): e72-e112. www.ncbi.nlm.nih.gov/pubmed/?term=Clin+Infect+Di…
Costantino, Thomas G., et al. “Randomized trial comparing intraoral ultrasound to landmark‐based needle aspiration in patients with suspected peritonsillar abscess.” Clinical Otolaryngology 38.3 (2013): 244-244. www.ncbi.nlm.nih.gov/pubmed/?term=Acad+Emerg+Med…
Menditto, Vincenzo G., et al. “Management of minor head injury in patients receiving oral anticoagulant therapy: a prospective study of a 24-hour observation protocol.” Annals of emergency medicine 59.6 (2012): 451-455. www.ncbi.nlm.nih.gov/pubmed/?term=Ann+Emerg+Med+…
Ray, Wayne A., et al. “Azithromycin and the risk of cardiovascular death.” New England Journal of Medicine 366.20 (2012): 1881-1890. www.ncbi.nlm.nih.gov/pubmed/?term=NEJM+(2012)+36…
Mourad, Ophyr, Valerie Palda, and Allan S. Detsky. “A comprehensive evidence-based approach to fever of unknown origin.” Archives of Internal Medicine 163.5 (2003): 545-551. www.ncbi.nlm.nih.gov/pubmed/?term=Arch+Intern+Me…
Kattwinkel, John, et al. “Part 15: neonatal resuscitation 2010 american heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care.” Circulation 122.18 suppl 3 (2010): S909-S919. www.ncbi.nlm.nih.gov/pubmed/20956432





Leave A Comment