Most Recent
Ep 106 Toxic Alcohols – Minding the Gaps
We see patients with toxic alcohol poisoning most commonly in three clinical scenarios. One, after an intentional suicide attempt where they tell you exactly what they took; two, when they come in agitated and won’t give you a history and the three, the inebriated patient found down. Alcohol is everywhere, and inevitably inebriated people show up at your ED with a myriad of medical and psychiatric problems. It’s our job as ED professionals, not only to identify traumatic, medical and psychiatric catastrophes in these patients but also to identify and manage the relatively rare but potentially life and sight threatening toxicologic diagnoses in the inebriated or agitated patient. And that isn’t so easy - especially when it comes to toxic alcohols. In this episode we help give you the knowledge of toxic alcohol poisoning recognition, clinical and lab clues, limitations of the osmolar gap, goals of management, time sensitive treatments and more...
BCE 65 Intimate Partner Violence – A Silent Epidemic
I was taken aback when I came across the statistic that approximately every 6 days a woman in Canada is killed by her intimate partner. Victims of intimate partner violence and domestic violence that we see in the ED typically involve an abuse story of repeated escalating violence over time that ends up in a crisis situation. The woman is often financially dependent on her abuser and has no one to turn to for help. In one of her worst cases ever from Janus General, Dr. Meeta Patel and I discuss the notions that Emergency providers have a unique opportunity to identify patients who are victims of intimate partner violence; that we should begin by thinking of how we can screen every woman of childbearing age about intimate partner violence in a private, safe and respectful way. We describe the quick Partner Violence Screen and finally how to offer supportive, empowering statements and connect your patients with resources like assaulted women’s helpline and shelters in your community...
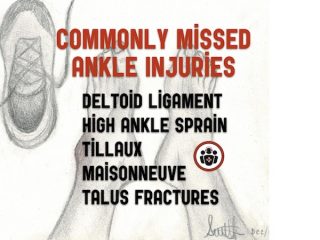
Ep 105 Commonly Missed Ankle Injuries
You probably can't remember the last time you worked a shift in the ED and didn’t see at least one patient with an ankle injury. While almost all of these patients are relatively straightforward to diagnose and manage a small but significant minority of these patients will have a more elusive diagnosis, that if not identified early, could lead to significant morbidity...
EM Cases Best of 2017 Top 10
Based on a blend of the number of podcast downloads, webpage views, social media engagement, number of positive emails and comments that I received, and my own favs, I'm pleased to bring you the EM Cases Best of 2017 Top 10. Many huge thanks to the entire EM Cases team, Advisory Board, SREMI, the amazing guest experts and you, the listeners of the podcasts, readers of the blogs, viewers of the videos and participants in the course, for making 2017 another successful year for EM Cases! And here they are...
WTBS 14 Improving Patient Flow in the ED: 7 Strategies for Nurses
It is both an evidence-based truth and almost a mantra of emergency department (ED) providers and leaders that the major cause of ED overcrowding is boarded patients. Yet 10 years of experience in more than 70 EDs has shown that impressive flow gains can be achieved despite a poor flow of admitted patients out of the ED. While I have always been and continue to be an advocate for improved admission processes and better ED resources, these issues should never excuse us from exploring our own role in improving flow in our departments. Fostering a culture in which all staff are committed to improving care through better flow will trump petty concerns about hierarchies and role descriptions—and it will improve morale.
Ep 104 Emergency Management of Intracerebral Hemorrhage – The Golden Hour
There exists a kind of self-fulfilling prognostic pessimism when it comes to ICH. And this pessimism sometimes leads to less than optimal care in patients who otherwise might have had a reasonably good outcome if they were managed aggressively. Despite the poor prognosis of these patients overall, there is some evidence to suggest that early aggressive medical management may improve outcomes. As such, the skill with which you manage your patient with ICH in those first few hours could be the most important determinant of their outcome. In this Golden Hour you have a chance to prevent hematoma expansion, stabilize intracerebral perfusion and give your patient the best chance of survival with neurologic recovery.