POCUS Cases Video Series has Launched!
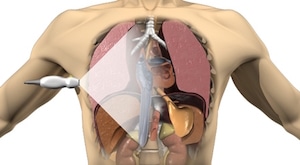
The long wait has been well worth it. The EM Cases POCUS Cases Video Series has officially been launched! POCUS Cases is an original EM Cases video series led by Dr. Robert Simard, an Emergency Physician at North York General Hospital and Sunnybrook Health Sciences Centre in Toronto. Rob always wished he had x-ray vision…but since he possesses no special powers…using Point-of-Care Ultrasound (POCUS) is the next closest thing. He completed a POCUS fellowship at NOSM and teaches POCUS nationally and internationally. He is the creator POCUS Cases, an original EM cases screencast that provides POCUS clinical pearls in an engaging and fun way that will help you provide stellar care to your patients...