Cardiovascular
Episode 20: Atrial Fibrillation
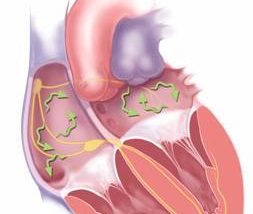
In this episode Dr. Clare Atzema, Dr. Nazanin Meshkat and Dr. Bryan Au discuss the presentation, etiology, precipitants, management and disposition of Atrial Fibrillation in the Emergency Department. The pros and cons of rate and rhythm control are debated, what you need to know about rate and rhythm control medications reviewed, and the strength of the Ottawa Aggressive Protocol discussed. The importance of appropriate anticoagulation is detailed, with a review of the CHADS-VASc score and whether to use Warfarin, Dabigatran or ASA for stroke prevention for patient with Atrial Fibrillation. We end off with a discussion on how to recognize and treat Wolff-Parkinson-White syndrome in the setting of Atrial Fibrillation.
Best Case Ever 7: Atrial Fibrillation
As a bonus to Episode 20 on Atrial Fibrillation, we present here, Dr. Clare Atzema, a leading EM researcher in Atrial Fibrillation, telling her Best Case Ever related to Afib. What would you do if you needed to cardiovert a patient who was too obese to fit on an ED stretcher? Dr. Atzema, along with Dr. Nazanin Meshkat and Dr. Bryan Au, discuss the presentation, etiology, precipitants, management and disposition of Atrial Fibrillation in the Emergency Department. The pros and cons of rate vs rhythm control are debated, what you need to know about Afib medications, and the value of the Ottawa Aggressive Protocol discussed. The importance of appropriate anticoagulation is detailed, with a review of the CHADS-VASc score and whether to use anticogulants or ASA for stroke prevention for patients with Afib. We end off with a discussion on how to recognize and treat Wolff-Parkinson-White syndrome in the setting of Atrial Fibrillation. [wpfilebase tag=file id=382 tpl=emc-play /] [wpfilebase tag=file id=383 tpl=emc-mp3 /]
Episode 15 Part 2: Acute Coronary Syndromes Management
In Part 2 of this Episode on Acute Coronary Syndromes Risk Stratification & Management, the evidence for various medications for ACS, from supplemental oxygen to thrombolytics are debated, and decision making around reperfusion therapy for STEMI as well as NSTEMI are discussed. Finally, there is a discussion on risk stratification of low risk chest pain patients and all it's attendant challenges as well as disposition and follow-up decisions. Dr. Eric Letovsky, the Head of the CCFP(EM) Program at the University of Toronto, Dr. Mark Mensour & Dr. Neil Fam, an interventional cardiologist answer questions like: What is the danger of high flow oxygen in the setting of ACS? When, if ever, should we be using IV B-blockers in AMI patients? How can you predict, in the ED, who might go on to have an urgent CABG, in which case Clopidogrel is contra-indicated? Which anticoagulant is best for unstable angina, NSTEMI and STEMI - unfractionated heparin (UFH), low molecular weight heparin (LMWH), or fonduparinux? Is there currenly any role for Glycoprotein 2b3a Inhibitors in ACS in the ED? When is thrombolysis better than PCI for STEMI? When should we consider facilitated angioplasty and rescue angioplasty? Which low risk chest pain patients require an early stress test? CT coronary angiography? Stress Echo? Admission to a Coronary Decision Unit (CDU)? and many more.......
Episode 15 Part 1: Acute Coronary Syndromes Risk Stratification
In Part 1 of this Episode on Acute Coronary Syndromes Risk Stratification Dr. Eric Letovksy, Dr. Mark Mensour and Dr. Neil Fam discuss common pearls and pitfalls in assessing the patient who presents to the ED with chest pain. They review atypical presentations to look out for, what the literature says about the value of traditional and non-traditional cardiac risk factors, the diagnostic utility of recent cardiac testing, and which patients in the ED should have a cardiac work-up. Finally, in the ED work up of Acute Coronary Syndromes Risk Stratification, they highlight some valuable key points in ECG interpretation and how best to use and interpret cardiac biomarkers like troponin. Drs. Letovksy, Mensour & Fam address questions like: How useful are the traditional cardiac risk factors in predicting ACS in the ED? How does a negative recent treadmill stress test, nuclear stress test or angiogram effect the pre-test probability of ACS in the ED? What does recent evidence tell us about the assumption that patients presenting with chest pain and a presumed new LBBB will rule in for MI and require re-perfusion therapy? How can we diagnose MI in the patient with a ventricular pacemaker? What is the difference between Troponin I and Troponin T from a practical clinical perspective? Is one Troponin ever good enough to rule out MI in the patient with a normal ECG? Should we be using a 2hr delta troponin protocol? How will the new ultra-sensitive Troponins change our practice? and many more.....
Best Case Ever 4 Acute Coronary Syndrome From Venous Source
In anticipation of Episode 15, 'Acute Coronary Syndromes' with Dr. Eric Letovsky, Dr. Mark Mensour and Dr. Neil Fam, we present here, Dr. Helman's 'Best Case Ever' of an ACS patient. In Episode 15: 'Acute Coronary Syndromes', Drs. Fam, Mensour , Letovsky and Helman discuss questions like: How does a recent negative stress test or angiogram effect the pre-test probability of ACS in the ED? What does recent evidence tell us about the assumption that patients presenting with chest pain and a presumed new LBBB will rule in for MI and require reperfusion therapy? [wpfilebase tag=file id=376 tpl=emc-play /] [wpfilebase tag=file id=377 tpl=emc-mp3 /]
Episode 12 Part 2: ACLS Guidelines – Atropine, Adenosine & Therapeutic Hypothermia
In Part 2 of this episode on ACLS Guidelines - Atropine, Adenosine & Therapeutic Hypothermia, Dr. Steven Brooks and Dr. Michael Feldman discuss the removal of Atropine from the PEA/Asystole algorithm, the indications and dangers of Adenosine in wide-complex tachycardias, pressors as a bridge to transvenous pacing in unstable bradycardias, and the key elements of post cardiac arrest care including therapeutic hypothermia and PCI. They answer questions such as: In which arrhythmias can Amiodarone cause more harm than good? Is there any role for transcutaneous pacing for asystole? When should Bicarb be given in the arrest situation? In what situations is Atropine contra-indicated or the dosage need to be adjusted? How has the widespread use of therapeutic hypothermia currently effected our ability to prognosticate post-arrest patients? What are the indications for PCI and thrombolysis in the cardiac arrest patient? Should we be using therapeutic hypothermia in the non-Vfib arrest patient? What is the best method for achieving the target temperature for the patient undergoing therapeutic hypothermia? and many more......