Topics in this EM Quick Hits podcast
Justin Morgenstern on imaging in renal colic patients (0:31)
Hanni Stoklosa on recognition and management of human trafficking (7:27)
Rohit Mohindra on management of atrial fibrillation in the COVID era (20:21)
Anand Swaminathan on transvenous pacemaker placement (24:48)
Rob Simard on COVID-19 lung POCUS (32:07)
Brit Long & Michael Gottlieb on COVID-19 dermatology (37:32)
Sarah Foohey & Paul Koblic on virtual simulation (44:29)
Podcast production and sound design by Anton Helman, voice editing by Sheza Qayyum
Podcast content, written summary & blog post by Graham Mazereeuw, edited by Anton Helman
Cite this podcast as: Helman, A. Swaminathan, A. Long, B. Gottlieb, M. Foohey, S. Koblic, P. Mohindra, R. Stoklosa, H. Simard, R. Morgenstern J. EM Quick Hits 20 – Imaging in Renal Colic, Human Trafficking, Atrial Fibrillation in COVID-19, Transvenous Pacemaker Placement, COVID-19 Lung POCUS, COVID-19 Dermatology, Virtual Simulation. Emergency Medicine Cases. June, 2020. https://emergencymedicinecases.com/em-quick-hits-20-june-2020/. Accessed [date].
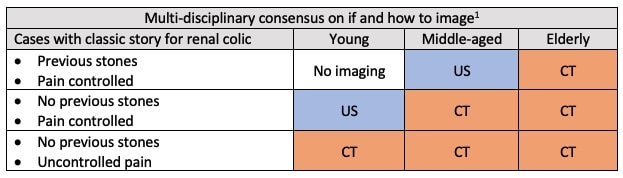
Imaging in renal colic
- Most cases do not require imaging
- Clear-cut indications for imaging:
- Worried about alternative diagnosis
- Febrile or septic
- Uncontrolled pain or urgent surgical intervention anticipated
- CT renal colic is the gold standard. However, less than 5% detect a clinically important alternative diagnosis and most CT scans do not change management
- POCUS is helpful: sensitivity is only 70%, specificity is 75% for all stones but POCUS is unlikely to miss large stones requiring surgical management
- Moore CL, Carpenter CR, Heilbrun ME, et al. Imaging in Suspected Renal Colic: Systematic Review of the Literature and Multispecialty Consensus. Ann Emerg Med. 2019;74(3):391-399.
- Smith-Bindman R, Aubin C, Bailitz J, et al. Ultrasonography versus computed tomography for suspected nephrolithiasis. N Engl J Med. 2014;371(12):1100-10.
Human Trafficking
- The ED is the front line for human trafficking: most trafficked persons access healthcare while being trafficked and they most commonly present to the ED
- Definition: a crime involving the recruitment, transportation, harbouring and/ or exercising control, direction or influence over the movements of a person in order to exploit that person, typically through sexual exploitation or forced labour
- Means of control can be force, fraud and/or coercion (psychological, financial, threats to person or family)
- Trafficked persons present with a variety of chief complaints: suicidal ideation, substance use, and illnesses of poor living conditions are common
- You have the skills to suspect that a person may be trafficked
- Vulnerable groups
- Under-regulated, underpaid industries
- Migrant workers
- Substance use/addiction (particularly opioids)
- Individuals experiencing homelessness
- Individuals supported through child welfare system
- LGBTQ youth
- Clues in the assessment
- History inconsistent with physical exam
- Patient is more fearful than expected
- Delayed presentation of common conditions
- Use the PEARR tool to foster safety and permit disclosure in your conversation
- Privacy: ensure patient privacy unless unsafe to do so
- Educate: educate patient about abuse and violence, available resources
- Ask: ask patient about their experiences
- Respect: respect patient wishes to disclose/not disclose
- Respond: as appropriate, provide resources
- Law enforcement: work with your patient to determine whether to involve law enforcement and which service to involve; Acting without their consent may harm them more than it helps
- Vulnerable groups
Dr. Stoklosa is on Twitter @hstoklosa
- Human Trafficking, Department of Justice, Government of Canada: https://www.justice.gc.ca/eng/cj-jp/tp/what-quoi.html
- PEARR Tool, Dignity Health: https://www.dignityhealth.org/hello-humankindness/human-trafficking/victim-centered-and-trauma-informed/using-the-pearr-tool
- Canadian Human Trafficking Hotline: https://www.canadianhumantraffickinghotline.ca/
- HEAL Trafficking: https://healtrafficking.org
Atrial Fibrillation in the COVID-19 Era
- Sedation for electrical cardioversion may necessitate aerosol-generating procedures, increasing the risk of SARS-CoV-2 transmission
- Consider cardioversion with procainamide 1 g IV over 1 hour (monitor for hypotension and QRS widening)
- Rate control: metoprolol 2.5-10 mg IV, repeated q15mins to a maximum of 15 mg plus metoprolol 25-50 mg PO loading dose if successful OR diltiazem 0.25 mg/kg IV plus a follow up dose of 0.15 mg/kg (caution is warranted if left ventricular function is unknown)
- Andrade JG, Verma A, Mitchell LB, et al. 2018 Focused Update of the Canadian Cardiovascular Society Guidelines for the Management of Atrial Fibrillation. Can J Cardiol. 2018;34(11):1371-1392.
Simplified Transvenous Pacemaker Placement
- Monitor heart rate using the O2 saturation monitor, instead of the ECG
- Line placement in the right internal jugular or the left subclavian vein provides the easiest approach to right side of heart
- Use a 5.5 Fr or 6 Fr catheter, bundled with your pacer line, as the standard 8 Fr introducer is too large
- Target a heart rate of 80 bpm – or at least 30 bpm faster than their present heart rate; turn the output all the way (~ 25 mA), with the sensitivity off (optimizing these settings allows wire placement to be the only variable in achieving capture)
- Advance the wire to 20 cm, then inflate the wire balloon to float it
- Mason, J. Placing a Transvenous Pacemaker. EM:RAP, October 2018. https://www.emrap.org/episode/transvenous/transvenous
- Sacchetti, A. Transvenous Pacemaker. EM:RAP, July 2019. https://www.emrap.org/episode/curbsideconsult2/curbsideconsult (subscribers only)
Lung POCUS and COVID-19
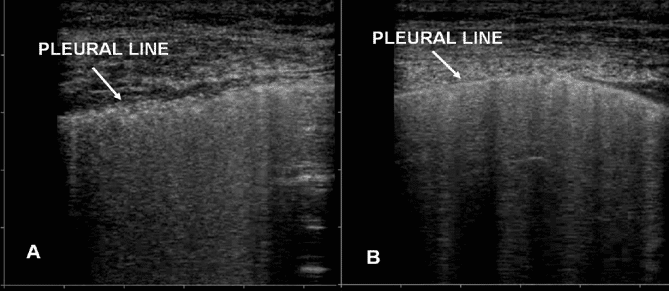
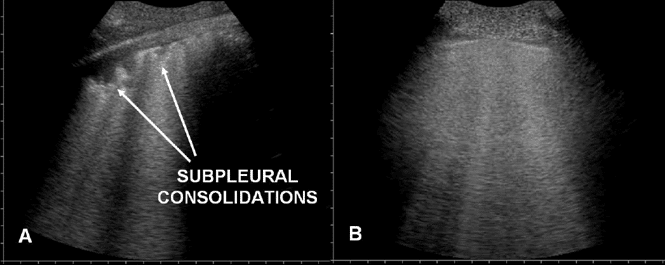
- Three key lung POCUS findings among patients with COVID-19
-
- Numerous B lines emanating from “lumpy, bumpy”, irregular pleura. This is consistent with non-cardiogenic pulmonary edema
- Sub-pleural consolidations, often bilateral, with a liver-like appearance (“hepatisation”) of the lungs (representing lobar pneumonia)
- Absence of pleural effusions
- Use dedicated COVID-19 POCUS machines; protect them and clean them as per local/national protocols.
- CXR may be more helpful/practical than POCUS in the diagnosis of COVID-19 pneumonia as x-ray has the advantage of not requiring patient contact
- Lung POCUS for COVID-19 pneumonia is unlikely to significantly aid in disposition decisions as disposition is based on vital sign abnormalities, work of breathing and social situation regardless of imaging findings
Figure 1. A) “lumpy, bumpy”, irregular pleura associated with non-cardiogenic pulmonary edema and COVID-19. B) Smooth, normal pleural line
Figure 2. A) Subpleural consolidations consistent with pneumonia and COVID-19. B) Normal lung appearance
- Rippey, J. Lung ultrasound: pneumonia. Life in the Fast Lane, December 2018 https://litfl.com/lung-ultrasound-pneumonia/
- Copetti R, Soldati G, Copetti P. Chest sonography: a useful tool to differentiate acute cardiogenic pulmonary edema from acute respiratory distress syndrome. Cardiovasc Ultrasound. 2008;6:16.
COVID-19 Dermatologic Complications
- Rashes may occur in up to 20% of patients with COVID-19 and may aid in the diagnosis
- Most dermatologic manifestations of COVID-19 are benign with the exception of that of distal ischemia
- Maculopapular rashes which may resemble pityriasis rosea
- Urticaria may affect a variety of locations of the body, but with sparing of the palm and soles and may be associated with more severe infection
- Vesicular rashes are similar to vesicles in chickenpox or disseminated zoster, but are a bit more scattered and discrete and less pruritic
- Petechiae and purpura are rare, but may be present with vasculitis or thrombocytopenia in the setting of COVID
- Chilblains most commonly affects the hands and feet, usually asymmetric red edematous +/- blistering, typically transient and affects younger patients
- Livedo racemosa is a web-like pattern of deep purple skin changes that can be diffuse, more commonly affects older patients, and may be associated with more severe infection
- Distal ischemia often begins as small, red or purple papules on the distal fingers and toes, becomes increasingly painful and eventually develops edema, bullae, and skin necrosis
- Recalcati S. Cutaneous manifestations in COVID-19: a first perspective [published online ahead of print, 2020 Mar 26]. J Eur Acad Dermatol Venereol. 2020;10.1111/jdv.16387. doi:10.1111/jdv.16387.
- Galván Casas C, Català A, Carretero Hernández G, et al. Classification of the cutaneous manifestations of COVID-19: a rapid prospective nationwide consensus study in Spain with 375 cases [published online ahead of print, 2020 Apr 29]. Br J Dermatol. 2020;10.1111/bjd.19163. doi:10.1111/bjd.19163
- Hedou M, Carsuzaa F, Chary E, Hainaut E, Cazenave-Roblot F, Masson Regnault M. Comment on “Cutaneous manifestations in COVID-19: a first perspective ” by Recalcati S [published online ahead of print, 2020 Apr 21]. J Eur Acad Dermatol Venereol. 2020;10.1111/jdv.16519. doi:10.1111/jdv.16519
- Tammaro A, Adebanjo GAR, Parisella FR, Pezzuto A, Rello J. Cutaneous manifestations in COVID-19: the experiences of Barcelona and Rome [published online ahead of print, 2020 Apr 24]. J Eur Acad Dermatol Venereol. 2020;10.1111/jdv.16530. doi:10.1111/jdv.16530
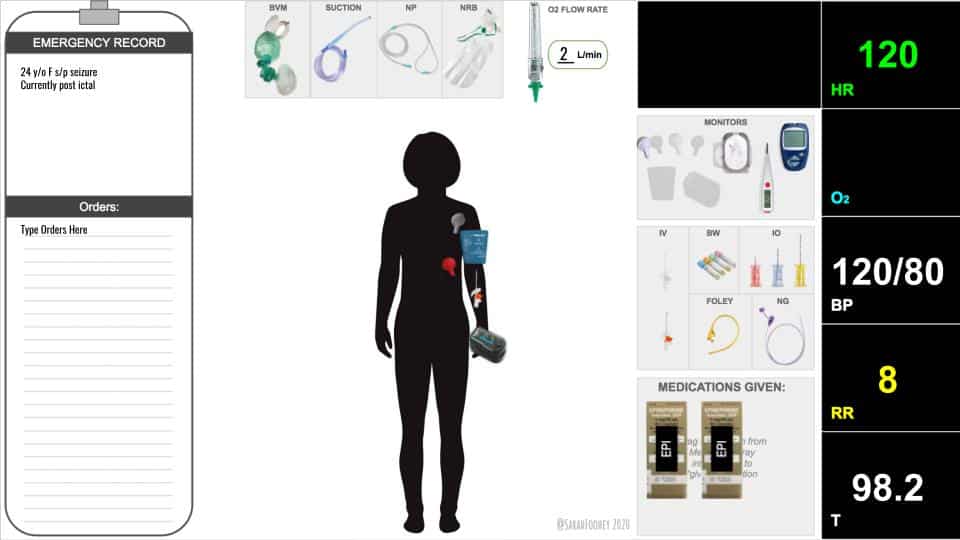
Virtual Simulation
- Virtual Resus Room
- Team members view and interact with a shared Google Slides document
- Interactive slides allow trainees to navigate the resus trays and equipment available to them in a resus room – they can be specific about their choices
- Modifiable slides allow trainees to demonstrate procedures in real time
- Hidden slides allow preceptors to introduce new elements or twists in the case
- Embedded videos show important physical exam findings (e.g. Kussmaul breathing in DKA)
- Teams communicate with audio and video, allowing communication in real time
- Navigating choices in equipment and procedures creates a cognitive load on trainees similar to that of a simulation lab
- Team Leaders develop delegation, management and communication skills in this dynamic environment
Dr. Foohey is on Twitter @SarahFoohey
Figure 1. Example of the virtual resus room
- Virtual Resus Room, https://virtualresusroom.com
None of the authors have any conflicts of interest to declare




[…] more about transvenous pacemaker placement at EM Quick Hits 20 (skip to […]