Topics in this EM Quick Hits podcast
Anand Swaminathan on 3-pronged approach to aortic dissection management (2:03)
Jonathan Wallace on rural practice tips for glue removal and ESP block for renal colic (9:06)
Sara Gray on everything you need to know about High Flow Nasal Cannula (15:21)
Maria Ivankovic on reducing the duration of antibiotic therapy (34:10)
Tahara Bhate on handover and learner oversight on QI corner (39:21)
Kerstin De Wit on the ADJUST-UNLIKELY tool for pulmonary embolism (49:13)
Podcast production, editing and sound design by Anton Helman
Podcast content, written summary & blog post by Anand Swaminathan, Sara Gray, Maria Ivankovic, Alex Chan edited by Anton Helman
Cite this podcast as: Helman, A. Swaminathan, A. Wallace, J. Gray, S. Ivankovic, M. Bhate, T. De Wit, K. EM Quick Hits 47 – HFNC, Dissection Drugs, Septic Arthritis, PE Testing, Antibiotic Course Length, Skin Glue Hacks, ESP Block. Emergency Medicine Cases. March, 2023 https://emergencymedicinecases.com/em-quick-hits-march-2023/. Accessed April 23, 2024.
Aortic Dissection 3-pronged approach to heart rate and blood pressure control
Aortic dissection is a hypertensive emergencies. Rapid control of both blood pressure and heart rate are essential to minimize extension of acute aortic dissection.
- Adequate analgesia: should be achieved before the diagnosis of aortic dissection is confirmed and before attempts at HR and BP control, to mitigate the contribution of catecholaminergic drive from pain to HR and BP
- Fentanyl 1mcg/kg q15-20 minutes
- Heart rate control: target HR 50-60BPM
- Esmolol (500-1000mcg/kilo) bolus followed by an infusion (50mcg/kg/min with reassessments every 5-10 minutes)
- Labetalol may be used as an alternative, which improves both HR and BP
- Blood pressure control: target SBP 90-100mmHg
- Nicardipine or Clovidipine are preferred agents if available
- Diltiazem 0.25-0.35mg/kg over 2 minutes, followed by a 5-10mg/hr infusion to target BP is acceptable as an alternative
- Nitroprusside may additionally be used though reflex tachycardia may be an issue
Episode 92 – Aortic Dissection Live from The EM Cases Course
ECG Cases 34 – ECG Interpretation in Aortic Dissection
- Hiratzka LF, Bakris GL, Beckman JA, et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease. Journal of the American College of Cardiology. 2010;55(14):e27-e129. doi:10.1016/j.jacc.2010.02.015
- Nienaber CA, Clough RE. Management of acute aortic dissection. The Lancet. 2015;385(9970):800-811. doi:10.1016/S0140-6736(14)61005-9
- Evangelista A, Isselbacher EM, Bossone E, et al. Insights From the International Registry of Acute Aortic Dissection: A 20-Year Experience of Collaborative Clinical Research. Circulation. 2018;137(17):1846-1860. doi:10.1161/CIRCULATIONAHA.117.031264
- Shimizu H, Fukui T, Tabata M, et al. Anti-impulse therapy for acute aortic dissection: a meta-analysis of current evidence. International Journal of Cardiology. 2016;223:47-50. doi:10.1016/j.ijcard.2016.08.254
- Erbel R, Aboyans V, Boileau C, et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. European Heart Journal. 2014;35(41):2873-2926. doi:10.1093/eurheartj/ehu281
Rural EM hacks for skin glue removal and ESP block
- Application of acetone or petroleum jelly (or petrolatum-based antibiotic ointment) can be used as accessible options for dissolving misapplied glue during laceration repairs, with the latter preferred for sensitive areas such as eyelids
- People who use cannabis daily may develop hyperalgesia and poor response to opioids which may require higher doses of opioids in the ED to achieve adequate analgesia
- For patients with renal colic in whom adequate analgesia cannot be achieved with medications, erector spinae block (ESP) may be an effective therapeutic strategy
- Coutts SJ, Sandhu R, Geh VSY. Tissue glue and iatrogenic eyelid gluing in children. Pediatric Emergency Care. 2012;28(8):810-811. doi:10.1097/pec.0b013e31826288fa
- Abrams DI, Couey P, Shade SB, et al. Cannabinoid-opioid interaction in chronic pain. Clin Pharmacol Ther. 2011;90(6):844-851. doi:10.1038/clpt.2011.188
- Karaca O, Pınar HU, Seyhan TO, et al. Comparison of ultrasound-guided erector spinae plane block and posterior quadratus lumborum block for the treatment of renal colic. Am J Emerg Med. 2021;43:231-235. doi:10.1016/j.ajem.2021.05.033
HFNC – High Flow Nasal Cannula – When, Why, Where, How & Why
- HFNC are nasal oxygen delivery devices that can deliver warmed and humidified oxygen with flows as high as 50-60L/min and FiO2 up to 100%, much higher compared to face mask
- HFNC is ideal for patients with:
- Acute respiratory failure
- Vomiting, claustrophobia, or intolerance to BiPAP or facemasks
- Septic patients with hypoxia – HFNC preferred over NIV (Surviving Sepsis Guidelines 2021)
- Patients who require advanced oxygen support that are not candidates for intubation
- HFNC is less/not useful in patients with:
- COPD, CHF, or severe asthma, where B-PAP/C-PAP likely to be more effective
- Upper airway obstruction such as epiglottitis, or croup
- How to identify patients that are likely to fail HFNC?
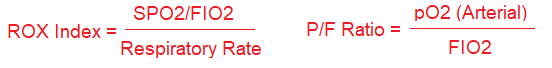
- Patients with high APACHE or SOFA score, low ROX index, or low improvement in P/F ratio pre and post HFNC are likely to fail HFNC and require intubation
-
- A ROX index >4 is reassuring as a predictor of HFNC success, and generally a ROX of >5 suggests that an ICU admission can most likely be avoided
- HFNC can be easily dialed in and adjusted
- Initial flow rate 30L/min, titrate in increased increments of 10L/min to target RR and work of breathing
- Titrate FiO2 to SpO2 of 92-96%
- When to abandon HFNC
- Worsening hypoxia or work of breathing
- Cardiac arrest
- Worsening LOC or aspiration or other indication for acute intubation
- Roca O, Caralt B, Messika J, et al. An Index Combining Respiratory Rate and Oxygenation to Predict Outcome of Nasal High-Flow Therapy. Am J Respir Crit Care Med. 2019;199(11):1368-1376
- Rochwerg B, Granton D, Wang DX, et al. High flow nasal cannula compared with conventional oxygen therapy for acute hypoxemic respiratory failure: a systematic review and meta-analysis. Intensive Care Med 2019; 45: 563–572
- Ou X, Hua Y, Liu J, et al. Effect of high-flow nasal cannula oxygen therapy in adults with acute hypoxemic respiratory failure: a meta-analysis of randomized controlled trials. CMAJ. 2017;189(7):E260-E267
- Ferreyro BL, Angriman F, Munshi L, et al. Association of Noninvasive Oxygenation Strategies With All-Cause Mortality in Adults With Acute Hypoxemic Respiratory Failure: A Systematic Review and Meta-analysis. JAMA. Published online June 04, 2020. doi:10.1001/jama.2020.9524
- Li J, Fink JB, Ehrmann S. High-flow nasal cannula for COVID-19 patients: low risk of bio-aerosol dispersion. Eur Respir J. 2020;55(5):2000892
- Mauri T, Turrini C, Eronia N, et al. Physiologic Effects of High-Flow Nasal Cannula in Acute Hypoxemic Respiratory Failure. Am J Respir Crit Care Med 2017; 195: 1207-1215
- Kang BJ, Koh Y, Lim CM, et al. Failure of high-flow nasal cannula therapy may delay intubation and increase mortality. Intensive Care Med 2015; 41:623
- Mauri T, Alban L, Turrini C, Cambiaghi B, Carlesso E, Taccone P, et al. Optimum support by high-flow nasal cannula in acute hypoxemic respiratory failure: effects of increasing flow rates. Intensive Care Med 2017;43(10):1453–63
- Kim SH, Kim CH, Kim SY, Song SH et al. Predicting factors for the failure of high flow nasal cannula therapy in patients with acute respiratory failure. European Resp Journal 2018;PA2297. DOI:1183/13993003.congress-2018.PA2297
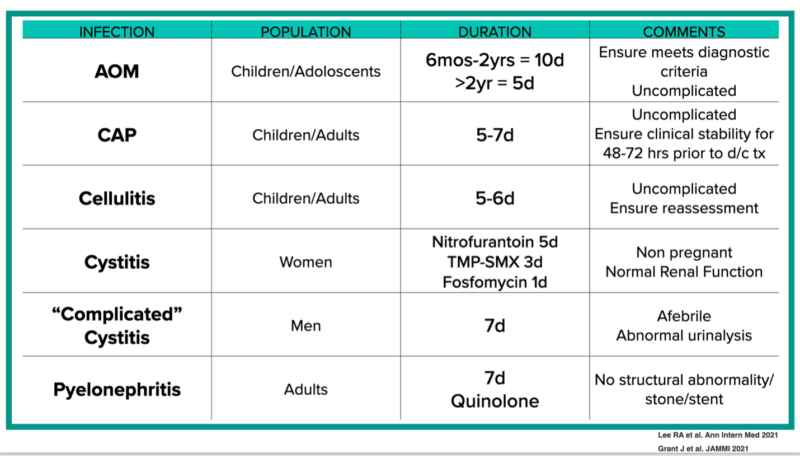
Antibiotic course duration – long antibiotic courses contribute to drug resistance and increased adverse events with no improvements in outcomes
- Antibiotic resistance is one of the greatest global health threats we face
- Shorter courses of antibiotics for uncomplicated bacterial infections are associated with both less resistance and adverse events, and are noninferior in terms of efficacy compared to longer courses
AMMI Practice Point: Duration of Antibiotic Therapy for Common Infections
- Grant J, Saux NL; members of the Antimicrobial Stewardship and Resistance Committee (ASRC) of the Association of Medical Microbiology and Infectious Disease (AMMI) Canada. Duration of antibiotic therapy for common infections. J Assoc Med Microbiol Infect Dis Can. 2021 Sep 30;6(3):181-197.
- Wald-Dickler N, Spellberg B. Short-course Antibiotic Therapy-Replacing Constantine Units With “Shorter Is Better”. Clin Infect Dis. 2019 Oct 15;69(9):1476-1479.
- https://www.ammi.ca/Content/Duration%20of%20Therapy%20nov%2024.pdf
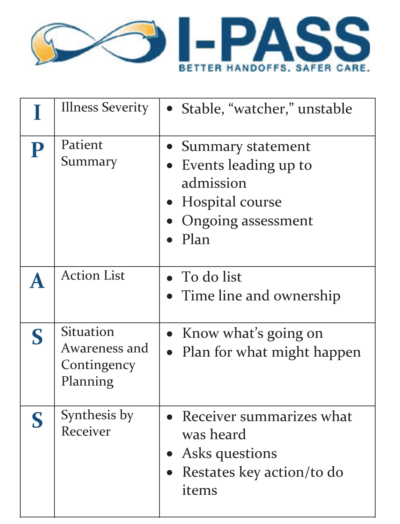
QI Corner – handover (handoff) pearls, degree of learner oversight, and the importance of re-assessments
- Recognize that the oversight of learners should be individualized to their level of training, strengths, and experience and develop a system that works for you to ensure that high-risk presentations are adequately assessed; training learners to have autonomy is also important
- When patients are examined in suboptimal conditions (such as in hallways during overcrowding), ensure that patient consent is obtained and documented
- Have a low threshold to reassess handover (or handoff) cases as a safety measure to both assess for clinical deterioration as well as missed diagnoses in initial assessment
Our recommended protocol for handover (handoff) is the I-PASS mnemonic
Please share your comments at the end of these show notes if you have any tips on how to balance appropriate learner oversight with learner autonomy
- Leonard M, Graham S, Bonacum D. The human factor: the critical importance of effective teamwork and communication in providing safe care. Qual Saf Health Care. 2004;13(Suppl 1):i85-i90.
- Blazin LJ, Sitthi-Amorn J, Hoffman JM, Burlison JD. Improving Patient Handoffs and Transitions through Adaptation and Implementation of I-PASS Across Multiple Handoff Settings. Pediatr Qual Saf. 2020 Jul 23;5(4):e323.
The Adjust-Unlikely tool to rule out pulmonary embolism

Source: cited article #2
- The Adjust-Unlikely strategy uses an age-adjusted D-dimer (age x 10 in patients older than 50) in cases where PE is not the most likely diagnosis and a threshold of 500ng/mL when it is, to decide if a CTPA is needed
- In one study, compared to the YEARS criteria, which had a sensitivity of 93% (95%CI 87-96) and a specificity of 45%, the Adjust-Unlikely tool had a sensitivity of 100% (95%CI 97.2-100) and a specificity of 32%
Episode 21: Pulmonary Embolism
Ep 113 Pulmonary Embolism Challenges in Diagnosis Part 1
Ep 114 Pulmonary Embolism Challenges in Diagnosis 2 – Imaging, Pregnancy, Subsegmental PE
- van der Hulle T, Cheung WY, Kooij S, et al. Simplified diagnostic management of suspected pulmonary embolism (the YEARS study): a prospective, multicentre, cohort study. Lancet. 2017;390(10091):289-297. doi:10.1016/S0140-6736(17)30885-1.
- de Wit K, Al-Haimus F, Hu Y, Ikesaka R, Chan N, Ibrahim Q, Klyn J, Clayton N, Germini F. Comparison of YEARS and Adjust-Unlikely D-dimer Testing for Pulmonary Embolism in the Emergency Department. Ann Emerg Med. 2022 Nov 10:S0196-0644(22)01118-0.
None of the authors have any conflicts of interest to declare





Leave A Comment