Topics in this EM Quick Hits podcast
Salim Rezaie on venous thromboembolism recurrence in subsegmental pulmonary embolism (1:23)
Andrew Petrosoniak on pain management in the polytrauma patient (6:44)
Nour Khatib on rural case on management of drowning patient (17:09)
Sara Reid on polio primer (24:30)
Anand Swaminathan on head-up cardiopulmonary resuscitation (32:20)
Podcast content, production, editing and sound design by Anton Helman
Podcast written summary & blog post by Raymond Cho, edited by Anton Helman
Cite this podcast as: Helman, A. Rezaie, S. Petrosoniak, A. Khatib, N. Reid, S, Swaminathan, A. EM Quick Hits 42 – Subsegmental PE, Trauma Analgesia, Drowning, Polio, Head-up CPR. Emergency Medicine Cases. September, 2022. https://emergencymedicinecases.com/em-quick-hits-42-september-2022/. Accessed April 25, 2024.
Best of REBEL EM: Venous thromboembolism recurrence in subsegmental pulmonary embolism
- The management of subsegmental PE is controversial as some believe anticoagulation is unnecessary, while others claim that there is a high risk of recurrence, necessitating the use of anticoagulation
- Clinical question: what is the risk of recurrent venous thromboembolism (VTE) in patients with subsegmental PE without DVT, without anticoagulation?
- SubSegmental Pulmonary Embolism Study (SSPE) is a multicenter prospective cohort study with 266 ED patients enrolled from 2011-2021; patients with newly diagnosed subsegmental PE were included while those with DVT, active cancer, history of VTE, supplemental O2 requirements, pregnant, already anticoagulated or hospitalized were excluded from the study; primary outcome was recurrent VTE within 90 days.
- 8/266 (3.1%, 95% CI 1.6-6.1%) patients had a recurrence of VTE, 4 with DVT and 4 with PE. 2 patients (0.7%, CI 0.2 – 2.9%) had major bleeding and 4 (1.4%, CI 0.6 – 4.0%) had minor bleeding.
- There was a higher than expected level of recurrent VTE but no patients with recurrent VTE had a fatal PE. The rate of major and minor bleeding was relatively low.
Bottom Line: In patients with isolated subsegmental PE without additional risk factors, it is reasonable to make a shared decision with the patient regarding anticoagulation based on this study.
Commentary: If a thrombosis/hematology or internal medicine clinic follow-up appointment within a week or two can be secured, it is reasonable to anticoagulate all patients with symptomatic subsegmental PE without contraindications to anticoagulation until their follow-up, as the risk of major bleeding when anticoagulated for only 1-2 weeks approaches zero.
- Le Gal G et al. Risk for Recurrent Venous Thromboembolism in Patients With Subsegmental Pulmonary Embolism Managed Without Anticoagulation: A Multicenter Prospective Cohort Study. Ann Intern Med. 2022.
- Propersi, M. (2022, July 28). VTE recurrence in Subsegmental PE: What’s the risk? REBEL EM – Emergency Medicine Blog. https://rebelem.com/vte-recurrence-in-subsegmental-pe-whats-the-risk/
Pain management in trauma

Source: Pain & Procedural Sedation in Acute Care. Reuben Strayer, Sergey Motov, & Lewis Nelson, eds.https://painandpsa.org/pain-in-the-poly-trauma-patient/
- Hicks, C., & Petrosoniak, A. (2017). Pain in the Polytrauma Patient. Pain and Procedural Sedation. https://painandpsa.org/pain-in-the-poly-trauma-patient/
- Motov, S., Mai, M., Pushkar, I., Likourezos, A., Drapkin, J., Yasavolian, M., Brady, J., Homel, P., & Fromm, C. (2017). A prospective randomized, double-dummy trial comparing IV push low dose ketamine to short infusion of low dose ketamine for treatment of pain in the ED. The American Journal of Emergency Medicine, 35(8), 1095-1100.
Rural EM Quick Hits Series: Management of drowning patients
- Background
- In drowning, water causes laryngospasm leading to hypoxia and respiratory failure/cardiac arrest
- Markers of poor outcomes include: 1. prolonged submersion time, 2. altered mental status, and 3. severe acidosis
- Management
- Initial assessment: GCS, rectal temperature, blood glucose, brief trauma survey
- Traditional ABC approach should be used (as opposed to CAB approach): supplemental O2 followed by BiPAP then intubation if patient fails to improve
- Manage hypothermia: patients with temperatures 28-32°C require active rewarming with forced air, radiant heat, and heat packs with goal to reach temperature > 34°C
- Identify potential causes for drowning, e.g. seizure, syncope, suicidal intent, etc.
- There is no role for routine administration of antibiotics
- Disposition
- Stable patients with GCS > 13, O2 > 95% RA, normal vitals, and clear lungs require 4-6 hours of monitoring before they can be safely discharged home
- Harries, M. (2003). Near drowning. BMJ, 327(7427), 1336-1338.
- Misch, M., Helman, A. CritCases 12 – Accidental Hypothermia and Cardiac Arrest. Emergency Medicine Cases. https://emergencymedicinecases.com/accidental-hypothermia-cardiac-arrest. Published January, 2019.
Polio primer – polio is back!
- Background – undervaccinated populations are at risk for paralytic polio
- Polio is an enterovirus spread via fecal-oral route with a 1-3 week incubation time, and communicability is highest at the time of symptom onset
- The oral polio vaccine contains an attenuated virus, which can be excreted into stool and transferred to other children; in rare cases and undervaccinated populations, this can spread continuously, allowing for mutation that may result in a strain with paralytic polio.
- The COVID pandemic has led to polio-undervaccinated populations in North America
- Clinical Features – a wide clinical spectrum
- Most patients are asymptomatic
- Mild disease: fever, fatigue, headache, and vomiting, which is self-limiting after a few days
- Moderate-to-severe disease: muscle pain, stiffness of back and neck +/- paralysis which usually onsets 1-3 weeks after infection. Recovery is possible but becomes increasingly irreversible with longer duration of paralysis.
- Acute paralytic polio: asymmetric paralysis that begins proximally then descends, with fever, meningeal irritation, bulbar involvement, reduced tone and loss of reflexes and sometimes muscle atrophy, flaccid paralysis, and respiratory insufficiency.
- Diagnosis in ED – acute flaccid paralysis + poor vaccination status = polio until proven otherwise
- Consider polio in anyone with acute weakness or flaccid paralysis in the context of incomplete or unvaccinated status and recent travel to areas with polio activity
- Lumbar puncture shows elevated CSF protein and pleocytosis
- 2 x Stool samples 24 hours apart for polio
- NP swab for polio
Bottom line: Polio is back due to undervaccinated populations in North America; consider polio in anyone with acute weakness or flaccid paralysis in the context of incomplete or unvaccinated status and recent travel to areas with polio activity
- Center for Disease Control. (2021, October 20). Poliovirus diagnostic methods. Centers for Disease Control and Prevention. https://www.cdc.gov/polio/what-is-polio/lab-testing/diagnostic.html
- Center for Disease Control. (2022, Aug 10). Poliomyelitis: For Healthcare Providers. Centers for Disease Control and Prevention. https://www.cdc.gov/polio/what-is-polio/hcp.html
- Howard, R. S. (2005). Poliomyelitis and the postpolio syndrome. BMJ, 330(7503), 1314-1318.
Head-up cardiopulmonary resuscitation
- The head/thorax are elevated slightly and compressions are administered in this position. Theoretically, this allows venous blood to drain from head to heart, which decreases ICP and increases cerebral blood flow.
- Recent evidence suggests that head-up CPR is associated with improved survival following out-of-hospital cardiac arrest (Moore et. al, 2022)
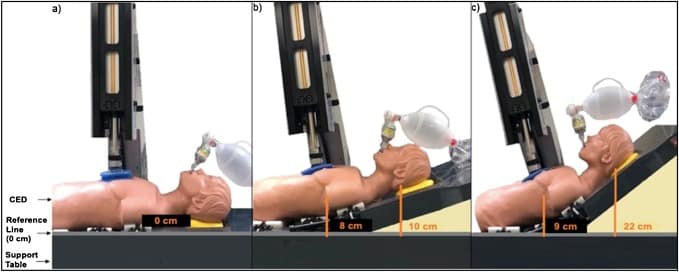
- This is a prospective registry study of 227 patients from 6 pre-hospital systems in the United States using active compression-decompression CPR, impedance threshold device and automated controlled elevation of the head and thorax (raises head to 22 cm and thorax to 9 cm); primary outcome was survival to hospital discharge, while secondary outcomes included ROSC and favorable neurologic survival; outcomes were compared to that of traditional CPR data from 3 large RCTs of high-performing prehospital systems.
- Heads-up CPR was associated with higher survival to hospital discharge when initiated in under 11 minutes (OR 3.28, 95% CI 1.55-6.92) but has lesser benefit when initiated later. This was also associated with higher probability of ROSC and favorable neurologic survival.
Bottom Line: There is promising data for head-up CPR, but is not yet ready for widespread implementation until an RCT is complete and there is thorough evaluation of costs associated with implementation.
Automated controlled elevation of the head and thorax (Source: Resuscitation, 2020)
- Moore, J. C., Pepe, P. E., Scheppke, K. A., Lick, C., Duval, S., Holley, J., Salverda, B., Jacobs, M., Nystrom, P., Quinn, R., Adams, P. J., Hutchison, M., Mason, C., Martinez, E., Mason, S., Clift, A., Antevy, P. M., Coyle, C., Grizzard, E., … Labarère, J. (2022). Head and thorax elevation during cardiopulmonary resuscitation using circulatory adjuncts is associated with improved survival. Resuscitation, 179, 9-17.
- Rezaie, S. (2021, May 1). In the pipeline: Head up CPR in OHCA? REBEL EM – Emergency Medicine Blog. https://rebelem.com/in-the-pipeline-head-up-cpr-in-ohca/
- Varney, J., Motawea, K. R., Mostafa, M. R., AbdelQadir, Y. H., Aboelenein, M., Kandil, O. A., Ibrahim, N., Hashim, H. T., Murry, K., Jackson, G., Shah, J., Boury, M., Awad, A. K., Patel, P., Awad, D. M., Rozan, S. S., & Talat, N. E. (2022). Efficacy of heads-up CPR compared to supine CPR positions: Systematic review and metaanalysis. Health Science Reports, 5(3).
None of the authors have any conflicts of interest to declare





Leave A Comment