Most Recent
Best Case Ever 42 Pediatric Cardiac Arrest
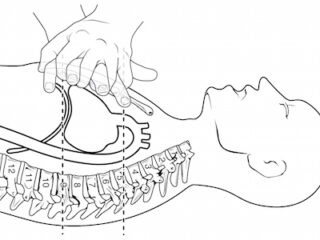
When was the last time you saw ventricular fibrillation in a 4 month old? Dr. Simard tells his Best Case Ever of a Pediatric Cardiac Arrest in which meticulous preparation, sticking to his guns, early activation of the transportation service, and clever use of point of care ultrasound helped save the life of a child. He explains the importance of debriefing your team after an emotionally charged case.
Episode 72 ACLS Guidelines 2015 Post Arrest Care
Once we've achieved ROSC our job is not over. Good post-arrest care involves maintaining blood pressure and cerebral perfusion, adequate sedation, cooling and preventing hyperthermia, considering antiarrhythmic medications, optimization of tissue oxygen delivery while avoiding hyperoxia, getting patients to PCI who need it, and looking for and treating the underlying cause. Dr. Lin and Dr. Morrison offer us their opinion on the new simplified approach to diagnosing the underlying cause of PEA arrests. We'll also discuss when it's time to terminate resuscitation or 'call the code' as well as some fascinating research on gender differences in cardiac arrest care. These co-authors of the guidelines will give us their vision of the future of cardiac arrest care and we'll wrap up the episode with a third opinion, so to speak: Dr. Weingart's take on the whole thing....
Episode 71 ACLS Guidelines 2015 – Cardiac Arrest Controversies Part 1
A lot has changed over the years when it comes to managing the adult in cardiac arrest. As a result, survival rates after cardiac arrest have risen steadily over the last decade. With the release of the 2015 American Heart Association ACLS Guidelines 2015 online on Oct 16th, while there aren’t a lot a big changes, there are many small but important changes we need to be aware of, and there still remains a lot of controversy. In light of knowing how to provide optimal cardio-cerebral resuscitation and improving patient outcomes, in this episode we’ll ask two Canadian co-authors of The Guidelines, Dr. Laurie Morrison and Dr. Steve Lin some of the most practice-changing and controversial questions.
Best Case Ever 41 Opiate Misuse and Physician Compassion
Opiate misuse is everywhere. Approximately 15-20% of ED patients in the US are prescribed outpatient opiates upon discharge. In Ontario, about 10 people die accidentally from prescription opiates every week. Between 1990 and 2010, drug overdose deaths in the US increased by almost four fold, eclipsing the rate of death from motor vehicle collisions in 2009. This was driven by deaths related to prescription opiates, which now kill more people than heroin and cocaine combined. Opiates are the most prescribed class of medication in the US. In 2010, one out of every eight deaths among persons aged 25 to 34 years was opiate-related. Four out of 5 new heroin users report that their initial drug was a prescription opiate. In Ontario, three times the people died from opiate overdose than from HIV in 2011. Yet, we are expected to treat pain aggressively in the ED. Dr. Reuben Strayer, the brains behind the fantastic blog EM Updates tells his Best Case Ever, in which he realizes the importance of physician compassion in approaching the challenging drug seekers and malingerers that we manage in the ED on a regular basis. This Best Case Ever is in anticipation of an upcoming main episode in which Dr. Strayer and toxicologist Dr. David Juurlink discuss how to strike a balance between managing pain effectively and providing the seed for perpetuating a drug addiction or feeding a pre-existing drug addiction, and how we best take care of our patients who we suspect might have a drug misuse problem.
Episode 70 End of Life Care in Emergency Medicine
Most of us in North America live in cultures that almost never talk about death and dying. And medical progress has led the way to a shift in the culture of dying, in which death has been medicalized. While most people wish to die at home, every decade has seen an increase in the proportion of deaths that occur in hospital. Death is often seen as a failure to keep people alive rather than a natural dignified end to life. This is at odds with what a lot of people actually want at the end of their lives: 70% of hospitalized Canadian elderly say they prefer comfort measures as apposed to life-prolonging treatment, yet as many as ⅔ of these patients are admitted to ICUs. Quality End of Life Care in Emergency Medicine is not widely taught. Most of us are not well prepared for death in our EDs – and we should be. There’s no second chance when it comes to a bad death like there is if you screw up a central line placement, so you need the skills to do it right the first time. To recognize when comfort measures and compassion are what will be best for our patients, is just as important as knowing when to intervene and treat aggressively in a resuscitation. Emergency physicians should be able to recognize not only the symptoms and patterns that are common in the last hours to days of life, but also understand the various trajectories over months or years toward death, if they’re going to provide the high quality end of life care that patients deserve. So, with the help of Dr. Howard Ovens, a veteran emergency physician with over 25 years of experience who speaks at national conferences on End of Life Care in Emergency Medicine, Dr. Paul Miller, an emergency physician who also runs a palliative care unit at McMaster University and Dr. Shona MacLachlan who led the palliative care stream at the CAEP conference in Edmonton this past June, we'll help you learn the skills you need to assess dying patients appropriately, communicate with their families effectively, manage end of life symptoms with confidence and much more...
WTBS 4 – Emergency Physician Speed: How Fast is Fast Enough?
Racing legend Mario Andretti famously said, “If everything seems under control, you’re just not going fast enough.” He was talking about cars, but to many beleaguered emergency physicians trying to keep up with the patient queue, emergency medicine often seems this way. This guest blog on emergency physician productivity began as a question to our national association, the Canadian Association of Emergency Physicians (CAEP): Are there any national standards with respect to emergency physician productivity, i.e., expected number of patients assessed per hour? The question was referred to the CAEP Public Affairs Committee and triggered a lively email discussion among our members....