In this ECG Cases blog we review 8 patients who presented with potential electrolyte emergencies. What does the ECG reveal, and how does this change management?
Written by Jesse McLaren; Peer Reviewed and edited by Anton Helman. November 2022
8 patients presented with potential electrolyte abnormalities. What does the ECG reveal, and how does this change management?
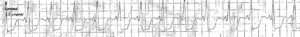
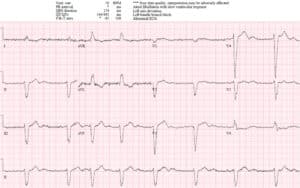
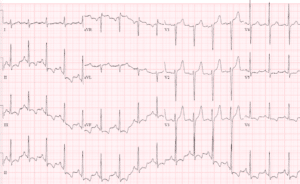
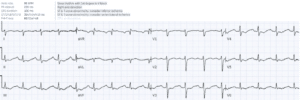
Case 1: 35yo history of type 1 diabetes and hypertension, with vomiting and glucose reading ‘high’. Old then new
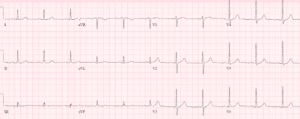
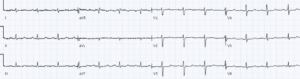
Case 2: 85 year old, history of Afib and chronic renal failure, with weakness, dysuria and fever. Old then new
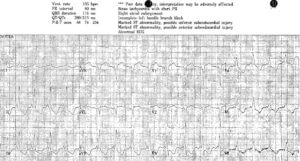
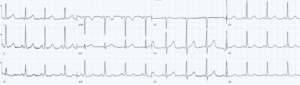
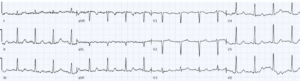
Case 3: 25 year old, history WPW and anorexia, with weight loss and weakness. EMS rhythm strip and triage ECG
Case 4: 20 year old, history renal tubal acidosis, with weakness and muscle cramps
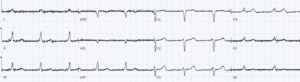
Case 5: 90yo history of AF and CHF on metalazone, with weakness and nausea. Old then new ECG
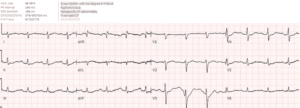
Case 6: 70 year old cancer patient on denosumab, with weakness. No cardiorespiratory symptoms. Old then new ECG
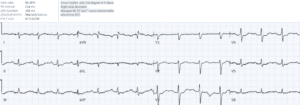
Case 7: 55 year old, dialysis patient, with weakness and paresthesias. Old then new ECG
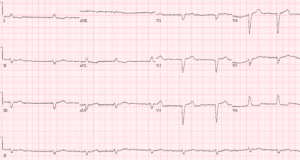
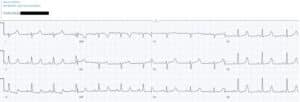
Case 8: 50 year old, history of alcohol use disorder, with weakness
ECG interpretation in electrolyte emergencies: Pretest, test & posttest
Pre-test: which patients are at risk for electrolyte emergencies?
Symptoms of electrolyte disturbances are often nonspecific, including weakness and GI symptoms, which can relate to the cause as well as the effect of the abnormality. But there are common risk factors that affect electrolyte homeostasis—including chronic medical conditions, acute illnesses, and medications—which can help generate a pre-test probability for an electrolyte emergency (including associated electrolyte abnormalities) and put the ECG in context [1]:
- Potassium is mainly intracellular, and regulation includes intake, shift to the intracellular space, and renal or GI excretion. So risk factors for hyperkalemia include potassium supplements, insulin deficiency, chronic or acute renal failure, or potassium sparing diuretics; risk factors for hypokalemia include malnutrition, increase insulin shifting, GI/renal losses, and concomitant hypomagnesemia. Patients in DKA are at risk for both hyperkalemia and iatrogenic hypokalemia.[2]
- Calcium is mainly stored in bone, and regulation includes intake, hormonal regulation (parathyroid hormone and vitamin D), bone resorption, and renal excretion. So risk factors for hypercalcemia include large intake of calcium and vitamin D, hyperparathyroidism, or metastatic cancer; risk factors for hypocalcemia include parathyroid or vitamin D deficiency, chronic renal failure, medications that interfere with calcium homeostasis, or critical illness (including sepsis, rhabdo, or massive transfusion).
- Magnesium is mainly intracellular, and regulation includes intake and renal excretion. So risk factors for hypermagnesemia include magnesium supplementation and chronic renal failure; risk factors for hypomagnesemia include malnutrition or diuresis, which can worsen concomitant hypokalemia.
Test: what look for on ECG?
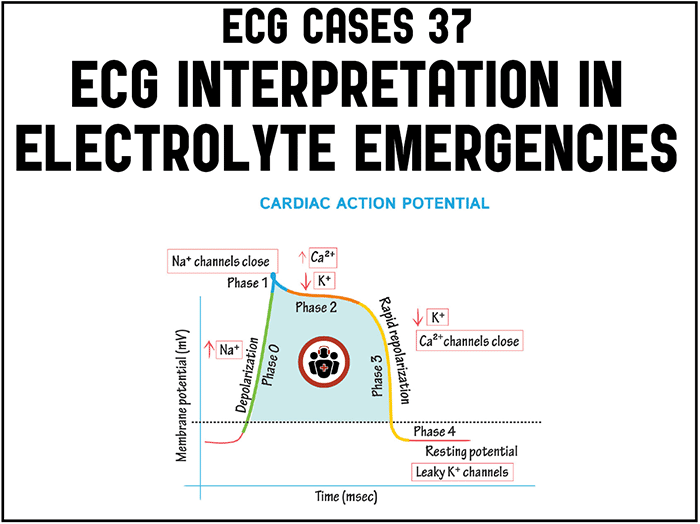
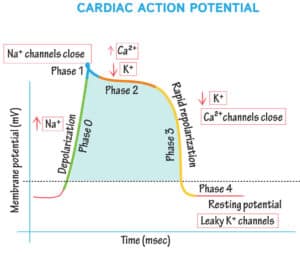
The cardiac action potential relies on flows of ions across the cardiomyocyte membrane. So electrolyte abnormalities can have serious cardiac manifestations, and IV electrolyte therapy can provide cardiac stabilization. Potassium affects the resting membrane potential, plateau phase of depolarization, and repolarization – so potassium abnormalities can have a variety of effects. Calcium affects the plateau phase (duration of ST segment), while magnesium can stabilize repolarization (shortening a prolonged QT interval).
- Hyperkalemia: the great imitator including bradycardia and junctional rhythms, wide PR and QRS, conduction blocks, axis deviation, ST elevation including Brugada phenocopy, and peaked T waves (narrow at the base and sharp at the peak). Greater number of abnormalities at higher levels, with risk of unstable bradycardia or wide complex rhythms. In patients with chronic renal failure, there may be long ST segment from concomitant hypocalcemia.
- Hypokalemia: tall P waves, diffuse ST depression with reciprocal ST-aVR, flat or inverted T waves and prominent U wave (long QU interval mistaken for long QT interval), and risk of ventricular arrhythmias. Or there may be additional long QT from associated hypomagnesemia.
- Calcium: inverse correlation with the ST segment – so hypercalcemia produces a short QT interval (from a short ST segment) and hypocalcemia produces a long QT interval (from a long ST segment).
- Hypomagnesium: associated with long QT interval, which predisposes to Torsades (polymorphic VT + long QT). There may be associated hypokalemia.
In other words, hypokalemia, hypocalcemia and hypomagnesemia all appear to prolong the QT interval, but they do so for different reasons: hypokalemia prolongs the QU interval which can be mistaken for the QT interval, hypocalcemia prolongs the ST segment (resulting in a long QT with a normal T wave), and hypomagnesemia prolongs the T wave (resulting in a long QT with a long T wave). Computer interpretation error includes confusing QU for QT interval or errors in measuring QT interval, so ECG interpretation should include an assessment of QT for computer accuracy, and manual measurement if needed: QT should be less than half the RR interval, which will overestimate at high rates and underestimate it at low rates,[6] corrected with Bazett’s formula: QTc = QT/ √ RR.
Post-test: how does the ECG change management?
If you suspect an electrolyte abnormality you’re going to measure the serum level and correct it if it is abnormal. So how does the ECG change management?
- Diagnosis: the ECG can help flag an abnormality that might not have been considered or included in routine blood work: for example, a short or long ST segment might alert to the possibility of a hyper or hypocalcemia and the need to measure extended electrolytes. Even if all electrolytes are measured, their serum level is not always reliable: magnesium serum levels are unreliable indicators of body stores, but a patient with a high pretest likelihood and ECG manifestation (eg alcohol use disorder with long QT) requires IV magnesium even with reassuring blood work.[3]
- Empiric treatment: while most electrolyte imbalances can wait for laboratory confirmation, patients with severe abnormalities are at risk for sudden decompensation before lab values return, and a quick ECG can guide empiric treatment and expedited tests. For example, in a study of severe hyperkalemia (≥6.5 mEq/L) in the ED, all adverse events had a preceding ECG showing hyperkalemic abnormalities but there was a delay to treatment until lab confirmation, and all adverse events happened prior to calcium administration.[4] So severe hyperkalemia is an ECG diagnosis that can trigger empiric IV calcium, and a stat VBG for confirmation. ECG abnormalities can also help avoid empiric treatment that may be harmful, eg giving insulin to DKA with hypokalemia, or giving QT prolonging medication to patient with long QT
- Prognosis: the ECG can help prognosticate electrolyte abnormalities and alert to the need for IV treatment. In a study of severe hypokalemia (≤2.5 mEq/L) in the ED, 30% of patients did not get an ECG and 40% did not get IV potassium replacement, while 77% of those who did get an ECG showed hypokalemic abnormalities.[5] This suggests that severe hypokalemia is under-treated even after being measured, and ECG interpretation can help highlight the dangerously low levels and the need for IV replacement.
Back to the cases
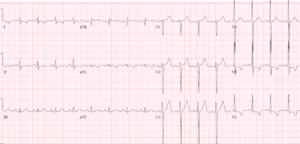
Case 1: hyperkalemia and pseudo-STEMI, treated empirically with calcium
- H: sinus tachycardia
- E: normal PR, nonspecific IVCD, normal QT
- A: new right axis
- R: slight delayed R wave progression
- T: pre-existing LVH
- S: peaked T waves and mild ST elevation
Impression: DKA with multiple signs of hyperkalemia, pseudo-STEMI. Treated empirically with calcium, with normalization of axis and return of T waves to baseline. Diagnosed with DKA and hyperkalemia (potassium 6.7).
Case 2: LBBB with hyperkalemia
- H: junctional rhythm
- E: wide QRS from pre-existing LBBB
- A: old left axis from LBBB
- R: old delayed R wave progression from LBBB
- T: normal voltages
- S: peaked T waves
Impression: acute on chronic renal failure with peaked T waves from hyperkalemia (6.5). Given calcium, insulin/D50 and fluids, and treated for urosepsis.
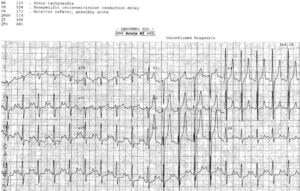
Case 3: severe hypokalemia mimicking subendocardial ischemia, treated empirically
- H: normal sinus
- E: short PR with delta and slurred QRS from WPW, normal QT, prominent U wave in V3
- A: normal axis
- R: normal R wave progression
- T: tall P waves inferior leads, normal QTS voltage
- S: diffuse ST depression with down-up T waves, with reciprocal STE-aVR
Impression: anorexia with multiple signs of hypokalemia, treated with empiric IV potassium and magnesium. Stat VBG confirmed potassium 1.9, normal serum magnesium. Discharge with after electrolyte replacement:
Case 4: hypokalemia, pseudo-long QT
- H: normal sinus
- E: prolong PR, normal QRS, normal QT (eg lead V2 T wave clearly visible with QT approx. 400)
- A: right axis
- R: normal R wave progression
- T: low voltages limb leads
- S: down/up ST segment and flat T wave
Impression: RTA with symptoms and ECG signs of hypokalemia (1.7). But QT is not prolonged: here is ECG repeated immediately, now with correctly calculated QT:
Treated with IV potassium and magnesium replacement. ECG repeated again, now K 2.4, with ongoing ST depression and down/up T waves:
ECG next day with potassium 3.5, with resolution of ST depression and now T waves upright:
Case 5: LBBB with hypokalemia
- H: atrial fibrillation with slow ventricular response
- E: wide QRS from LBBB, normal QT, prominent U wave (seen inferiorly, and V4-5). QT seems long in V6 but V4-5 shows this is from long QU
- A: old left axis from LBBB
- R: old delayed R wave from LBBB
- T: normal voltages
- S: discordant and proportional ST changes
Impression: patient with weakness on metalazone with prominent U waves from severe hypokalemia (1.9mEq/L); also severely hyponatremic (110) without ECG manifestations
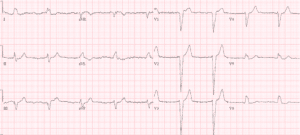
Case 6: hypocalcemia from denosumab
- H: normal sinus
- E: normal PR/QRS, long QT from long ST
- A: normal axis
- R: early R wave
- T: normal voltages
- S: incidental S1Q3T3
Impression: weakness on denosumab with long ST segment. Diagnosed with severe hypocalcemia (1.25), treated with IV calcium.
Case 7: dialysis patients with combined hyperkalemia and hypocalcemia
- H: normal sinus rhythm
- E: normal PR/QRS/QT but prolonged ST segment
- A: new right axis
- R: normal R wave progression
- T: normal voltages
- S: peaked T waves
Impression: dialysis patient with ECG evidence of combined hyperkalemia (7.1mEq/L), and hypocalcemia (1.85: normal 2.2 – 2.62). Treated with calcium and then dialysis
Case 8: hypomagnesemia
- Heart rate/rhythm: borderline sinus tach
- Electrical intervals: normal PR/QRS, prolonged QT (correctly measured by computer)
- Axis: normal
- R-wave progression: normal
- Tall/small voltages: normal voltages
- ST/T: flat T wave
Impression: alcohol use disorder with prolonged QT interval, at risk of polymorphic VT. Empirically treated with IV magnesium. Potassium level was normal, Magnesium not as low as ECG suggested (0.65mmol/L, with normal 0.7-1.1). Resolution of prolonged QT and normalization of T waves:
Take home points on ECG interpretation in electrolyte emergencies
- Hyperkalemia – bradycardia/blocks, wide PR/QRS and peaked T waves, multiple abnormalities indicate a critically high level: empiric calcium and stat VBG
- Hypokalemia – diffuse ST depression, down-up T waves, prominent U waves with a long QU interval (mimicking prolonged QT), and associated hypomagnesemia: empiric magnesium, stat VBG
- Calcium – long or short ST segments can indicate low or high calcium levels, respectively: confirmation by extended electrolytes
- Hypomagnesemia – associated with long QT which can be out of proportion to serum levels: empiric magnesium if QTc>500
- QT interval can be misinterpreted by computers: verify the QT for accuracy and consider causes of apparent lengthening – including hypokalemia (long QU), hypocalcemia (long ST), and hypomagnesemia (long QT)
References for ECG Cases 37 – ECG interpretation in electrolyte emergencies
- Diercks DB, Shumaik GM, Harrigan RA, et al. Electrocardiographic manifestations: electrolyte abnormalities. J of Emerg Med 2004;27(2):153-160
- Arora S, Cheng D, Wyler B, et al. Prevalence of hypokalemia in ED patients with diabetic ketoacidosis. Am J Emerg Med 2012;30:481-484
- Reinhart R. Magnesium deficiency: recognition and treatment in the emergency medicine setting. Am J Emerg Med 1992;10(1):78-83
- Durfey N, Lehnhof B, Bergeson A, et al. Severe hyperkalemia: can the electrocardiogram risk stratify for short-term adverse events. West J of Emerg Med 2017 Aug;18(5):963-971
- Makinouchi R, Machida S, Matsui K et al. Health Sci Rep 2020 May;5(3):e594
- Berling I, Isbister GK. The half RR rule: a poor rule of thumb and not a risk assessment tool for QT interval prolongation. Acad Emerg Med 2015;22:1139-1144







Thank you