Most Recent
POCUS Cases 10 Limitations, Pitfalls and Accuracy of POCUS for Ruptured AAA
Dr. Rob Simard discusses one of the most important uses of POCUS in the ED, and that is for AAA. He reviews the literature on the accuracy of POCUS for AAA as well as demonstrates the limitations and the common pitfalls in this POCUS Cases video....
EM Quick Hits 26 LAST, Sodium Nitrite Poisoning, Post-intubation Care, Tetracaine for Corneal Abrasion, ST Segment in Occlusion MI, Coping with COVID
Anand Swaminathan on LAST prevention, recognition and management, Emily Austin on sodium nitrite suicide kit poisoning, methemoglobinemia and methylene blue, Hans & Erin Rosenberg on post-intubation analgesia and sedation, Salim Rezaie on short-term tetracaine for corneal abrasions new evidence, Jesse MacLaren on differentiating ST deviation in occlusion MI from other causes, Robert Maunder on a 3 step approach to coping and building resilience during the COVID pandemic...
POCUS Cases 9 Abdominal Free Fluid in Trauma
Rob Simard explains how to incorporate abdominal POCUS into your assessment of the trauma patient, he reviews the literature on accuracy of POCUS for assessment of abdominal free fluid, reviews the key POCUS steps and cautions us about interpretation of your findings in trauma patients who have sustained an injury to their abdomen...
Ep 152 The 7 Ts of Massive Hemorrhage Protocols
Dr. Jeannie Callum, Dr. Andrew Petrosoniak and Dr. Barbara Haas join Anton in answering the questions: How do you decide when to activate the MHP? How do you know when it is safe to terminate the MHP? What lab tests need to be done, how often, and how should the results be shared with the clinical team? Once the dust settles, what do we need to tell the patient and/or their family about the consequences of being massively transfused? What should be the lab resuscitation targets? Why is serum calcium important to draw in the ED for the patient who is exsanguinating? How do we mitigate the risk of hypothermia? What can hospitals do to mitigate blood wastage? If someone is on anti-platelets or anticoagulants what is the best strategy to ensure the docs in the ED know what to give and how much? Until the results of lab testing come back and hemorrhage pace is slowed, what ratio of plasma to RBCs should we target? What's better, 1:1:1 or 2:1:1? Should we ever consider using Recombinant Factor 7a? If the fibrinogen is low, what is the optimal product and threshold for replacement? When and how much TXA? Anyone you wouldn’t give it to? and many more...
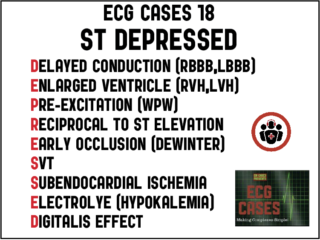
ECG Cases 18 – ST DEPRESSED Mnemonic and Occlusion MI
In this ECG Cases blog we look at 10 patients who presented with potentially ischemic symptoms and ST depression. Which had occlusion MI?
EM Quick Hits 25 Cerebral Venous Thrombosis, Diphenhydramine Alternatives, Abdominal Compartment Syndrome, Neonatal Constipation, Intubating Metabolic Acidosis
In this month's EM Quick Hits podcast: Justin Morgenstern on which patients to consider cerebral venous thrombosis in, Maria Ivankovic on diphenhydramine alternatives, Brit Long on abdominal compartment syndrome, Sarah Reid on neonatal "constipation" - when to worry, and Anand Swaminathan on intubating the patient with metabolic acidosis...