In this ECG Cases blog we look at 10 patients who presented with potentially ischemic symptoms and ST depression. Which had occlusion MI?
Written by Jesse McLaren; Peer Reviewed and edited by Anton Helman. February 2020
10 patients presented with potentially ischemic symptoms and ST depression. Which had occlusion MI?
Case 1: 75yo with one day of shortness of breath and diaphoresis. HR 110, BP 120. Old then new ECG
Case 2: 55yo prior CABG with one hour of chest pain. HR 40, BP 80/40. Old then new ECG
Case 3: 20yo with syncope, HR 50 BP 120/60
Case 4: 60yo with one hour of chest pain and shortness of breath. Normal vitals. Serial ECGs
Case 5: 50yo with one hour of chest pain. Normal vitals
Case 6: 75yo with one hour of chest pain. Normal vitals. Serial ECGs
Case 7: 60yo with one hour of palpitations. HR 150, BP 130/70
Case 8: 50yo exertional chest pain resolved with rest. Normal vitals
Case 9: 50yo CAD on ASA/plavix with weakness and presyncope, no chest pain like prior MI. HR 100, BP 110/50. Old then new ECG
Case 10: 35yo with one day of vomiting and weakness
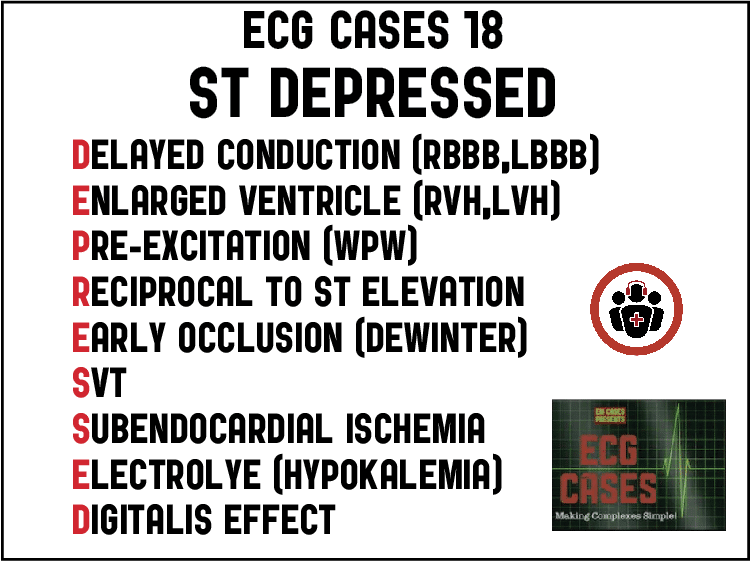
ST ‘DEPRESSED’ mnemonic and occlusion MI
As a review of ST depression explained, “In many instances, STD is associated with acute coronary syndromes (ACS)—both acute ischaemia and acute infarction; this electrocardiographic pattern, however, may also be found in patients with non-ischaemic events, such as left bundle branch block (LBBB), left ventricular hypertrophy (LVH), and those with therapeutic digitalis levels. Proper interpretation of the ECG in these patients will assist the clinician in arriving at the correct diagnosis—in effect, separating acute coronary syndrome from the non-ischaemic, more ‘benign’ causes of STD”[1]
Step 1: Differentiate ST depression that is secondary to abnormal conduction (bundle branch block, ventricular hypertrophy, or pre-excitation) from primary ST depression.
Step 2: Determine the cause within these two broad categories. This approach, and differential, is summarized by the mnemonic ‘DEPRESSED’:
Secondary to abnormal conduction
- Delayed conduction (RBBB, LBBB/paced)
- Enlarged ventricle (LVH, RVH)
- Pre-excitation (WPW)
Primary: acute coronary occlusion
- Reciprocal to ST elevation
- Early occlusion (deWinter T wave)
Primary: supply/demand mismatch
- SVT (rate related)
- Subendocardial ischemia (including non-occlusive MI, massive GI bleed, PE, sepsis)
Primary: metabolic/medication
- Electrolye (hypokalemia)
- Digitalis
Like the differential for ST elevation, there can be baseline secondary ST depression with superimposed primary changes—which disproportionate ST changes can help identify (eg modified Sgarbossa criteria for LBBB, or concordant/disproportionate ST changes in RBBB). While the STEMI paradigm dichotomizes ST elevation and ST depression, early occlusion can manifest as ST depression only (eg. DeWinter T waves with ST depression and hyperacute T waves), and both ST elevation and depression can co-exist in the same ECG and represent the same current of injury. As a couple of cardiologists explained a decade ago, “the STEMI and non‐STEMI differentiation ignores one of the basic tenets of electrocardiography, that is, that any deflection will produce a reciprocal image 180 degrees removed, on the opposite aspect of the field. (Contemplation of V1 and V6 in the setting of bundle branch block or of ventricular hypertrophy should make this concept abundantly clear.) In simple terms, during myocardial infarction, ST elevation or depression are in fact identical entities, that is, a result of an injury current viewed from opposite aspects of the electric field of the heart.”[2]
In some cases of occlusion MI (OMI) the reciprocal ST depression is more obvious than the ST elevation. In inferior OMI, ST depression in aVL can highlight subtle inferior ST elevation and/or hyperacute T waves. In posterior OMI, reciprocal ST depression isolated to the anterior leads can be more obvious than the small degree of ST elevation on the posterior leads. On the other hand, ST elevation in aVR is not “STEMI-equivalent” but is reciprocal to diffuse ST depression—with a broad differential including baseline LVH, subendocardial ischemia (from non-occlusive MI, PE, sepsis or GI bleed) or OMI.
So the real question is not whether it’s a “STEMI” or “NonSTEMI” but what is the cause of the ST changes, and whether it reflects OMI (i.e. total or near-total occlusion with insufficient collaterals, leading to rapid myocardial necrosis) or a non-occlusive MI (NOMI). As a new study found, only 60% of OMIs met STEMI criteria, and the 40% of STEMI(-)OMI had delays to reperfusion and adverse outcomes more similar to STEMI(+)OMI than NOMIs[3].
Back to the cases
Case 1: LBBB with STEMI(-)OMI(+)
- Heart rate/rhythm: sinus tach
- Electrical conduction: new LBBB
- Axis: normal
- R-wave: delayed R wave progression from LBBB
- Tension: can’t assess LVH
- ST/T changes: concordant STD in V3 (Sgarbossa) and disproportionately discordant STD in V4 (STD/R wave>0.30, modified Sgarbossa)
Impression: “new LBBB” is not an indication for cath lab activation, but this ECG was diagnostic of LBBB + OMI, missed by computer and physician until patient had VF arrest. Cath lab activated after ROSC: 95% circumflex occlusion, peak troponin I = 50,ooo ng/L
Case 2: RBBB with STEMI(-)OMI(+)
- H: junctional and sinus bradycardia
- E: old RBBB
- A: right axis
- R: tall R wave in V1 from RBBB
- T: no hypertrophy
- S: deep ST depression in anterior leads
Impression: high likelihood of OMI based on prior CABG presenting with chest pain and hemodynamic instability (which is itself an indication for the cath lab), confirmed on ECG. Despite dramatic reciprocal ST depression in anterior leads, there was only minimal ST elevation on posterior leads (below) but the cath lab was still activated: 100% occlusion of circumflex graft, first Trop I was negative but peak was 50,000, followed by cardiac arrest.
Case 3: HOCM
- H: sinus bradycardia
- E: normal intervals
- A: normal axis
- R: large voltages with late transition
- T: LVH
- S: secondary ST changes including STE/TWI anteriorly, and STD inferolaterally
Impression: young person with syncope and significant LVH with secondary repolarization abnormalities. HOCM on echo.
Case 4: WPW + inferoposterior STEMI(-)OMI
- H: normal sinus
- E: first ECG has short PR with delta wave from WPW, resolved on second
- A: normal axis
- R: first ECG has tall R wave in V1 from WPW, second has early R wave transition (R>S in V2) from posterior MI
- T: no hypertrophy
- S: first ECG has anterior STD secondary to WPW, second has anterior STD from posterior MI, and inferior STE + reciprocal change in aVL from inferior MI
Impression: WPW concealing infero-posterior MI, which became apparent when the conduction normalized on the repeat ECG. While there is only STE and hyperacute in lead III, there is reciprocal STD/TWI in aVL confirming inferior MI, and tall R wave with STD in V2-3 indicating posterior involvement. Cath lab activated: 100% RCA occlusion, first Trop I was 50 and peak 24,000 ng/L. Discharge ECG had resolution of inferior STE and anterior STD, and inferior reperfusion T wave inversion:
Case 5: inferoposterior STEMI(-)OMI(+)
- H: normal sinus
- E: normal conduction
- A: normal axis
- R: early transition (R>S in V2)
- T: no hypertrophy
- S: STD/TWI in I/AVL is reciprocal to minimal concave STE in III/aVF, and STD in V2-3 with TWI in V2 is reciprocal to minimal posterior STE (15 lead below)
Impression: inferoposterior OMI, more obvious on reciprocal antero-lateral STD than infero-posterior STE. Cath lab activated: 100% RCA occlusion, first Trop I was negative, peak 50,000 ng/L. Discharge ECG had resolution of STE/STD/TWI, and reperfusion T wave inversion inferiorly:
Case 6: lateral STEMI(-)OMI(+)
- H: normal sinus, one PVC in first ECG
- E: normal conduction
- A: left axis
- R: normal R wave progression
- T: borderline LVH
- S: >1mm STE in V6 only, but are evolving deWinter T waves contiguously (especially in V4), and mild straightening STE in I/aVL highlighted by reciprocal STD in III/aVF
Impression: lateral OMI. Cath lab activated: 99% occlusion of first diagonal. First Trop I was 200 and peak 8,000 ng/L. Discharge ECG had reperfusion T wave inversion in lateral leads, and resolved inferior reciprocal change
Case 7: SVT
- H: SVT
- E: no visible P waves
- A: normal axis
- R: normal R wave progression
- T: no hypertrophy
- S: inferolateral STD
Impression: SVT with rate-related inferolateral STD, which resolved after cardioversion:
Case 8: NOMI
- H: sinus brady with PAC
- E: normal conduction
- A: normal axis
- R: delayed R wave transition (R>S only at V5)
- T: no hypertrophy
- S: mild inferolateral STD, not reciprocal to any anterior STE or hyperacute T waves
Impression: resolved anginal symptoms with mild ST depression, not reciprocal to any hyperacute T waves or STE. Appropriately admitted for non-urgent angiography, which revealed a non-occlusive thrombus causing a small MI: 90% circumflex lesion, peak Trop I of 200 ng/L. Discharge ECG had improvement of mild ST changes:
Case 9: patient returned with subendocardial ischemia from GI bleed
- H: borderline sinus tach
- E: normal conduction
- A: normal axis
- R: normal progression
- T: no hypertrophy
- S: diffuse STD with reciprocal STE in aVR
Impression: if treated as “STEMI-equivalent” this patients would have received heparin and nitro for a GI bleed. But this diffuse STD represents subendocardial ischemia which has a broader differential. The symptoms were different from the patient’s recent MI and there was no clear cause on POCUS so they were fluid resuscitated. Lab returned showing significant hemoglobin drop from GI bleed. Discharge ECG had resolution of diffuse ST depression:
Case 10: hypokalemia
- H: sinus brady
- E: prominent U waves seen inferiorly
- A: normal axis
- R: normal R wave progression
- T: no hypertrophy
- S: diffuse ST depression with mild reciprocal STE in avR
Impression: diffuse STD with prominent U waves in patient with vomiting and weakness. Potassium 2.2. Changes resolved after potassium replacement:
Take home points for ST DEPRESSED mnemonic and occlusion MI
- Consider the differential when you see ST segments that are ‘DEPRESSED’: Delayed conduction (BBB), Enlarged ventricle (hypertrophy), Pre-excitation (WPW), Reciprocal to ST elevation, Early occlusion (deWinter T wave), SVT, Subendocardial ischemia, Electrolyte (hypokalemia), or Digitalis effect
- Baseline secondary ST changes can have superimposed primary ischemic changes, eg LBBB + modified Sgarbossa
- Reciprocal ST depression can be more obvious than STE (eg posterior OMI), or can serve to highlight subtle STE and hyperacute T wave (eg inferior OMI)
References
- Pollehn T, Brady WJ, Perron AD, et al. The electrocardiographic differential diagnosis of ST segment depression. Emerg Med J 2002 Mar;19(2):129-35.
- Phibbs B, Nelson W. Differential classification of acute myocardial infarction into ST- and non-ST segment elevation is not valid or rational. Ann of Noninvas Electrocardiol 30 June 2010,15(3):191-99.
- Meyers HP, Bracey A, Lee D, et al. Comparison of the ST-elevation myocardial infarction (STEMI) vs. NSTEMI and Occlusion MI (OMI) vs NOMI paradigms of acute MI. J of Emerg Med 2020 Dec 8;S0736-4679(20)31070-2.


























Absolutely amazing! Please keep posting these wondering tutorials!
It will be of a great help if this is available as a downloadable PDF.Thanks.