In this main episode podcast, Dr. David Carr joins Anton to give us his simplified approach to syncope based solely on history, physical and ECG to help guide disposition decisions. We answer questions such as: What features have the best likelihood ratios to help distinguish syncope from seizure? What key clinical features on history and physical exam can help us distinguish orthostatic and reflex syncope from the more sinister cardiac syncope? What is the best approach to ECG interpretation for the patient who has presents with syncope? Are syncope clinical decision tools any better than physician gestalt? and many more….
Podcast production, sound design & editing by Anton Helman; voice editing by Braedon Paul
Written Summary and blog post by Kate Dillon, edited by Anton Helman August, 2022
Cite this podcast as: Helman, A. Carr, D. Syncope Simplified. Emergency Medicine Cases. August, 2022. https://emergencymedicinecases.com/simplifying-syncope. Accessed April 23, 2024
The ED approach to syncope is almost entirely based on a focused but thorough history, cardiac physical exam and ECG rather than laboratory tests and imaging. The first step is distinguishing syncope from seizure. The next step is distinguishing cardiac from non-cardiac syncope. Our ultimate aim is to make safe disposition decisions based on this approach.
Distinguishing syncope from seizure based on history
The most useful symptoms reported by patient/witness for identifying seizure
- Head turning during event – sensitivity 43%; specificity 97%; LR 14
- Unusual posturing during the event – sensitivity 35%; specificity 97%; LR 13
- Absence of presyncope – sensitivity 77%; specificity 86%; LR 5.6
- History of epilepsy – more likely seizure
- Post-ictal state – 96% of patients with seizures
- Urinary incontinence – sensitivity 24%; specificity 96%; LR 6.7 *despite this impressive LR, urinary incontinence cannot reliably distinguish syncope from seizure
The most useful findings evaluated by the physician for identifying patients with seizures:
- The presence of a cut tongue – sensitivity 45%; specificity 97%; LR 17
- Lateral tongue bite has a 100% specificity for tonic clonic seizure
- Patient has no recall of unusual behaviors before the loss of consciousness – sensitivity 53%; specificity 87%; LR 4.0
The most useful symptoms reported by patient or witness for identifying patients with syncope:
- Loss of consciousness with prolonged sitting or standing (sensitivity 40%; specificity 98%; LR 20
- Dyspnea before loss of consciousness (sensitivity 24%; specificity 98%; LR 13
- Palpitations before loss of consciousness (sensitivity 34%; specificity 96%; LR 8.3
- Muscle tone (increased tone more likely seizure, decreased tone more likely syncope)
- Number of limb jerks – The 10:20 Rule: patients with witnessed <10 myoclonic jerks after sudden loss of consciousness is more like syncope vs >20 myoclonic jerks is more likely seizure
Clinical Pitfall: Even though the +LR for urinary incontinence increases the likelihood of seizure, urinary incontinence cannot reliably distinguish seizure from syncope and should not be relied on to do so.
Clinical Pearl: Lateral tongue bite after sudden loss of consciousness has a 100% specificity for tonic clonic seizure.
Clinical Pearl: Approximately 90% of people who have a syncopal episode will have myoclonic jerks, the 10:20 Rule to help determine whether syncope or seizure is more likely. If there are <10 jerks it is more likely to be syncope, if you have >20 jerks it is more likely to be a seizure.
Distinguishing cardiac syncope from non-cardiac syncope
After considering syncope caused by diagnoses that typically present with additional clinical features (eg vascular catastrophes such as subarachnoid hemorrhage, ectopic pregnancy, massive GI bleed, ruptured AAA etc) the priority in the ED should be distinguishing cardiac syncope from non-cardiac syncope.
Categories of syncope
- Reflex syncope – vasovagal, carotid sinus syndrome, situational
- Orthostatic syncope – drug induced, volume depletion, neurogenic
- Cardiovascular syncope – mechanical (PE, tamponade, aortic stenosis), dysrhythmias
Cardiac syncope clinical clues
- Cardiovascular risk factors
- Structural heart disease (especially HCM, aortic stenosis)
- Pacemaker
- Sudden syncope with no prodrome
- Exertional syncope
- Prodrome that includes palpitations, shortness of breath or chest pain
- Associated facial injury (including dental injury, eye glasses damage, tip of tongue bite)
- Family history of unexplained sudden death, drowning or single MVC <50 years of age
- Aortic stenosis murmur – high mortality rate in patients with critical aortic stenosis and syncope
Clinical Pearl: when asking about a family history of premature sudden death, also ask about unexplained drownings or single vehicle collisions, as these might point to an underlying inheritable cardiac cause
Clinical Pearl: older patients with aortic stenosis, a valve diameter <1cm and a syncopal episode have very poor prognosis, and high mortality rate – so use your stethoscope and auscultate the chest; an aortic valve repair can be life-saving in this setting
Clinical Pitfall: do not assume that a patient who has a pacemaker has orthostatic or reflex syncope; their pacemaker needs to be interrogated
Reflex Syncope
Clinical clues – prodrome of feeling warm/nausea, history of recurrent syncope after an unpleasant sight, sound, smell or pain, prolonged standing, during a meal, being in crowded/hot places, autonomic activation (carotid sinus massage/shaving, pressure on the eye/ocular-bradycardic reflex, micturition, defecation).
Physical Exam – despite reports from the cardiology literature stating that carotid sinus massage is useful in patients with unexplained syncope, our expert does not see a role for carotid sinus massage to diagnosis reflex syncope in the ED.
Eagle’s Syndrome – a rare but morbid cause of reflex syncope
While the vast majority of reflex syncope etiologies are benign, Eagle’s Syndrome is a rare cause of syncope that involves a calcified, elongated stylohyoid ligament that presses on the carotid during neck extension and can lead to syncope, tinnitus and throat pain or mimic stroke syndromes/dissection. It is identified on CT scan. Surgical management can prevent further syncopal episodes.
Clinical Pearl: Eagle’s Syndrome is a rare cause of syncope that involves a calcified, elongated stylohyoid ligament that presses on the carotid during neck extension and can lead to syncope; in patients who present with recurrent syncope after activities that involve neck extension (eg car mechanic, yoga, star-gazing etc) with associated tinnitus or throat pain, consider a CT of the neck to rule out Eagle’s syndrome.
Orthostatic Syncope
Clinical Clues – prodrome of lightheadedness after changing from lying/sitting to sitting/standing position, post-prandial hypotension, temporal relationship with start or change of dosage of vasoactive drugs/diuretics, autonomic neuropathy (diabetes, Parkinsonism), volume losses.
Clinical Pitfall: a common pitfall is assuming that the cause of syncope is orthostatic and failing to search further for cardiac causes in older patients who are found to have an orthostatic drop. Orthostatic vital signs do not predict 30 day serious outcomes in older emergency department patients with syncope. Many older patients will have an orthostatic drop at baseline, and some patients with orthostatic symptoms will not have an orthostatic drop; orthostatic vitals are non-specific and may lead to premature closure

Source: Alboni P, Brignole M, Menozzi C, et al. Diagnostic value of history in patients with syncope with or without heart disease. J Am Coll Cardiol. 2001;37(7):1921-1928.
Is presyncope less morbid than syncope in older patients?
The differential for patients with pre-syncope and syncope are the same. Older patients with syncope or pre-syncope have comparable 1-month risk of major adverse cardiac events.
REBEL EM review of outcomes in syncope vs. pre-syncope
Simple 7-step approach to ECG interpretation for syncope
ECGs are the most important test in patients with syncope, and in many cases of discrete syncope without other symptoms, an ECG is the only test required in the ED. It is important to scrutinize the rhythm strip or 12-lead ECG from EMS as it may reveal a transient cardiac dysrhythmia that does not appear on the ED ECG.

Approach to ECG interpretation for patients who present with syncope (Source: David Carr by personal correspondence)
1.Brady- or tachydysrhythmias – including heart blocks, ventricular tachycardia etc – these are usually obvious
2.Hypertrophic Cardiomyopathy (HCM): inheritable cardiac condition, number one cause of sudden death in young athletes (1:500 prevalence)
a) Voltage criteria for LVH in precordial and limb leads
b) Narrow, “dagger-like” Q waves in inferior and lateral leads

Source: Life in the Fast Lane blog
3.Wolf-Parkinson-White (WPW): short PR, delta wave (upsloping QRS)

Source: https://www.healio.com/cardiology/learn-the-heart/ecg-review/ecg-topic-reviews-and-criteria/wpw-review
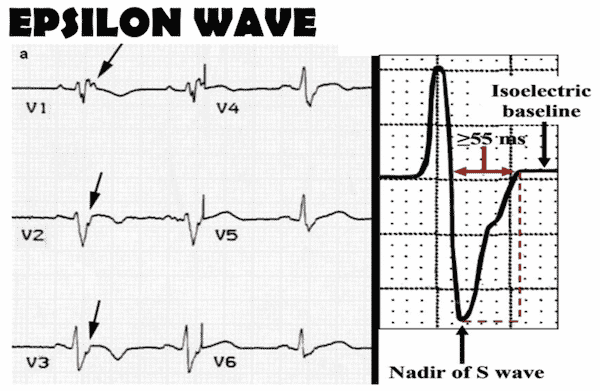
4. Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC): T-wave inversion in V1,V2, V3 (unlike Wellen’s that is V1-V4), epsilon wave (looks like a reverse delta wave, with slurring of the downstroke of the QRS, from the nadir of the S wave to the isoelectric line +/- a notch)
5.Brugada – down-sloping ST elevation in V1/2

Source: https://medschool.co/tests/ecg-disease-patterns/brugada-syndrome
Clinical Pearl: Brugada often comes out when people are febrile and more arrhythmogenic, so think about this in patient with fever and palpitations and make sure you take a close look at the ECG – remember if you miss Brugada, the person has a 10% chance of death in the next year
ECG Cases in depth review and examples of Brugada: ECG diagnosis of Brugada
6. Long QT
7. Bifascicular block (especially in the presence of a first-degree block) in a patient with syncope are at high risk of degenerating into 3rd-degree block and often require a pacemaker
Clinical pearl: one can cover most of ECG interpretation in the patient with syncope by simply looking for any abnormalities in the ECG intervals – PR, QRS and QT; this covers heart blocks, WPW, wide QRS tachydysrhythmias, HCM, Long QT syndrome and short QT syndrome
ECG Cases: ECGs in Cardiac Syncope
Is routine blood work necessary for patients who present to the ED with syncope?
In our expert’s view there is limited value in “routine” labs in patients deemed to be low-risk by physician gestalt. While troponins are often drawn in patients with syncope, evidence suggests that Troponin testing should be reserved for patients in whom the clinician suspects ACS and not drawn routinely in patients who present to the ED with syncope. Patients in whom labs should be considered:
- Suspect a bleed (CBC +/- coags)
- Suspect a PE (Dimer/CTPA)
- Suspect/possible pregnancy (B-HCG)
- Suspect an electrolyte abnormality based on medication change/ECG (lytes, extended lytes)
- Suspect ACS (i.e., chest pain or equivalent – troponin)
To image, or not to image: The value of CT head and PoCUS in syncope
Patients with clear cardiac syncope or reflex syncope do not routinely require a CT head. Imaging should be considered when secondary causes of syncope are suspected such as subarachnoid hemorrhage and vertebrobasilar “drop” attack stroke, and when non-trivial head injury as a result of the syncopal episode is suspected. Remember that for a CNS lesion to cause syncope directly, it needs to either effect both cerebral hemispheres or the brain stem.
Similarly, PoCUS should be considered when secondary causes of syncope are suspected, such as AAA, PE, aortic dissection or when major trauma results from the syncopal episode.
Which patients with syncope require a work up for pulmonary embolism?
Surprisingly, the PESIT trial, an observational study out of Italy found a 17.3% rate of PE in patients presenting to the ED with a first-time episode of syncope. This study had many limitations, and a subsequent North American prospective, multicenter, cohort study demonstrated a 30-day PE prevalence of only 0.6%. While PE can cause syncope and these patients are at high risk for poor outcomes, PE should not be routinely worked up for syncope patients. If there are significant findings on history, physical, ECG that suggest PE, then a work up should be considered based on validated decision tools. In our expert’s opinion there is no role for routinely ordering a D-Dimer for patients who present to the ED after a syncopal episode.
Are clinical decision tools better than physician gestalt for determining low risk syncope for safe discharge?
Decision-making tools, despite their varying level of external validation, can be used to reassure clinicians and assist in shared decision-making when considering safe discharge of patients who have presented to the ED after a syncopal episode. The San Francisco Syncope Rule (SFSR) requires a hematocrit, and is the easiest to remember at the bedside, but sensitivity for adverse events was poor in external validation studies, and sensitivity 86% and 87% and specificity 49% and 52% in two meta-analyses.
The Canadian Syncope Risk Score (CSRS) requires a troponin level (see above for value of troponin in syncope) and has shown excellent sensitivities in internal validation studies. Scores of -2 or higher were found to have sensitivity 99% and specificity of 26%. Scores of -1 or higher had sensitivity 98%, specificity 46%. On secondary internal validation in Canada, patients with very low and low risk scores had 0.3% and 0.7% risks of a serious outcome. However, a recent external validation in Italy demonstrated that the CSRS is no better than physician gestalt at predicting outcomes for patients with syncope. Additionally, physician gestalt had a lower rate of adverse events compared to low-risk patients on the CSRSP. Physician gestalt is incorporated into the score which may limit its usefulness.
In our expert’s opinion physician gestalt based on a focused but thorough clinical assessment should be used to identify low risk patients who are safe for discharge from the ED. Syncope decision tools can be used to reassure physicians and patients in shared decision making.
Additional outpatient testing for low-risk patients with syncope
For patients discharged from the ED in whom there is some suspicion for a cardiac cause of syncope, referral to a cardiologist/internist for further work up may be warranted (i.e., Holter, loop recorder, ECHO etc.). The yield of Holter monitoring in patients with syncope may be as low as 1-2% in an unselected population. In general, external loop recorders have a higher diagnostic yield than Holter monitoring. It is our expert’s opinion that decisions about which outpatient tests are performed are best left to the consultant.
References
-
- Albassam OT, Redelmeier RJ, Shadowitz S, Husain AM, Simel D, Etchells EE. Did This Patient Have Cardiac Syncope? JAMA. 2019;321(24):2448.
- Sheldon R, Rose S, Ritchie D, et al. Historical criteria that distinguish syncope from seizures. J Am Coll Cardiol. 2002;40(1):142-148.
- Brigo F, Nardone R, Ausserer H, Storti M, Tezzon F, Manganotti P, Bongiovanni LG. The diagnostic value of urinary incontinence in the differential diagnosis of seizures. Seizure. 2013 Mar;22(2):85-90.
- Pottkämper JCM, Hofmeijer J, van Waarde JA, van Putten MJAM. The postictal state – What do we know? Epilepsia. 2020 Jun;61(6):1045-1061.
- Benbadis SR, Wolgamuth BR, Goren H, Brener S, Fouad-Tarazi F. Value of tongue biting in the diagnosis of seizures. Arch Intern Med. 1995 Nov 27;155(21):2346-9.
- Shmuely S, Bauer PR, van Zwet EW, van Dijk JG, Thijs RD. Differentiating motor phenomena in tilt-induced syncope and convulsive seizures. Neurology. 2018 Apr 10;90(15):e1339-e1346.
- Alboni P, Brignole M, Menozzi C, et al. Diagnostic value of history in patients with syncope with or without heart disease. J Am Coll Cardiol. 2001;37(7):1921-1928.
- Taniguchi T, Morimoto T, Shiomi H, Ando K, Kanamori N, Murata K, Kitai T, Kawase Y, Izumi C, Kato T, Ishii K, Nagao K, Nakagawa Y, Toyofuku M, Saito N, Minatoya K, Kimura T; CURRENT AS Registry Investigators. Sudden Death in Patients With Severe Aortic Stenosis: Observations From the CURRENT AS Registry. J Am Heart Assoc. 2018 May 18;7(11):e008397.
- Saccomanno S, Greco F, DE Corso E, Lucidi D, Deli R, D’Addona A, Paludetti G. Eagle’s Syndrome, from clinical presentation to diagnosis and surgical treatment: a case report. Acta Otorhinolaryngol Ital. 2018 Apr;38(2):166-169.
- Sutton R. Carotid sinus syndrome: Progress in understanding and management. Glob Cardiol Sci Pract. 2014 Jun 18;2014(2):1-8.
- White JL, Hollander JE, Chang AM, Nishijima DK, Lin AL, Su E, Weiss RE, Yagapen AN, Malveau SE, Adler DH, Bastani A, Baugh CW, Caterino JM, Clark CL, Diercks DB, Nicks BA, Shah MN, Stiffler KA, Storrow AB, Wilber ST, Sun BC. Orthostatic vital signs do not predict 30 day serious outcomes in older emergency department patients with syncope: A multicenter observational study. Am J Emerg Med. 2019 Dec;37(12):2215-2223.
- Bastani A, Su E, Adler DH, et al. Comparison of 30-Day Serious Adverse Clinical Events for Elderly Patients Presenting to the Emergency Department With Near-Syncope Versus Syncope. Ann Emerg Med. 2019;73(3):274-280. doi:10.1016/j.annemergmed.2018.10.032
- Brignole M, Moya A, de Lange FJ, et al. 2018 ESC Guidelines for the diagnosis and management of syncope. European Heart Journal. 2018;39(21):1883-1948. doi:10.1093/eurheartj/ehy037
- Chiu DT, Shapiro NI, Sun BC, Mottley JL, Grossman SA. Are Echocardiography, Telemetry, Ambulatory Electrocardiography Monitoring, and Cardiac Enzymes in Emergency Department Patients Presenting with Syncope Useful Tests? A Preliminary Investigation. The Journal of Emergency Medicine. 2014;47(1):113-118. doi:10.1016/j.jemermed.2014.01.018
- CT Head in Syncope (ChoosingWisely Canada) https://choosingwiselycanada.org/recommendation/emergency-medicine/
- Goyal N, Donnino MW, Vachhani R, Bajwa R, Ahmad T, Otero R. The utility of head computed tomography in the emergency department evaluation of syncope. Internal and Emergency Medicine. 2006;1(2):148-150.
- Hatharasinghe AT, Etebar K, Wolsky R, Akhondi H, Ayutyanont N. An Assessment of the Diagnostic Value in Syncope Workup: A Retrospective Study. HCA Healthcare Journal of Medicine. 2021;2(6). doi:10.36518/2689-0216.1306
- Pournazari P, Oqab Z, Sheldon R. Diagnostic Value of Neurological Studies in Diagnosing Syncope: A Systematic Review. Canadian Journal of Cardiology. 2017;33(12):1604-1610.
- Lindner G, Pfortmueller CA, Funk GC, Leichtle AB, Fiedler GM, Exadaktylos AK. High-Sensitive Troponin Measurement in Emergency Department Patients Presenting with Syncope: A Retrospective Analysis. PLoS One. 2013 Jun 18;8(6):e66470.
- Sandhu RK, Raj SR, Thiruganasambandamoorthy V, et al. Canadian Cardiovascular Society Clinical Practice Update on the Assessment and Management of Syncope. Canadian Journal of Cardiology. 2020;36(8):1167-1177.
- Shen WK, Sheldon RS, Benditt DG, et al. 2017 ACC/AHA/HRS Guideline for the Evaluation and Management of Patients With Syncope: Executive Summary. J Am Coll Cardiol. 2017;70(5):620-663.
- Prandoni P, Lensing AW, Prins MH, Ciammaichella M, Perlati M, Mumoli N, Bucherini E, Visonà A, Bova C, Imberti D, Campostrini S, Barbar S; PESIT Investigators. Prevalence of Pulmonary Embolism among Patients Hospitalized for Syncope. N Engl J Med. 2016 Oct 20;375(16):1524-1531.
- Thiruganasambandamoorthy V et al. Prevalence of Pulmonary Embolism Among Emergency Department Patients with Syncope: A Multicenter Prospective Cohort Study. Ann Emerg Med 2019.
- Solbiati M, Talerico G, Villa P, et al. Multicentre external validation of the Canadian Syncope Risk Score to predict adverse events and comparison with clinical judgement. Emergency Medicine Journal. 2021;38(9):701-706.
- Thiruganasambandamoorthy V, Rowe BH, Sivilotti MLA, et al. Duration of Electrocardiographic Monitoring of Emergency Department Patients with Syncope. Circulation. 2019;139(11):1396-1406.
- Sivakumaran S, Krahn AD, Klein GJ, et al. A prospective randomized comparison of loop recorders versus Holter monitors in patients with syncope or presyncope. The American Journal of Medicine. 2003;115(1):1-5.
Drs. Helman and Carr have no conflicts of interest to declare
Now test your knowledge with a quiz.




I’m going to give this a dead heat tie alongside hyponatremia for the best EM cases episode ever.
Thanks for the feedback. From an excellent clinician like you Dr Venugopal this means a lot
Serial Orthostatic Changes are Relevant .
Example patient on near maximal reduced ejection failure heart failure therapy may become volume depleted .
Also with the SGLT2 in hot weather there will be pre-syncope and syncope .
Diabetics will develop autonomic neuropathy and if they exercise you need to record supine and string blood pressure .
Don’t under-do Hb in Elderly on NSAIDs and aspirin as regards GI bleeds and anticoagulants .
Hyponatremia is common .
Excellent pod cast
I just stated as ANP gerontology, syncope clinic and this was so interesting and enjoyable to listen to on long train journey
Many thanks