In this ECG Cases blog we look at 10 patients who presented with ST elevation, and review the differential diagnosis of ST elevation using the ELEVATIONS mnemonic. Which had occlusion MI?
Written by Jesse McLaren; Peer Reviewed and edited by Anton Helman. January 2021
Ten patients presented with potentially ischemic symptoms and ST elevation. Which had Occlusion MI (OMI)?
Case 1: 40yo ESRD with weakness, nausea/vomiting. AVSS
Case 2: 70yo with three days of shortness of breath. Hypertensive with borderline sats
Case 3: 90yo with 9 hours of chest pain and diaphoretic. HR 100, BP 100
Case 4: 30yo with presyncope. AVSS
Case 5: 55yo with 4 hours of chest pain. AVSS
Case 6: 45yo with 3 hours of chest pain. AVSS
Case 7: 40yo with 7 hours of chest pain. AVSS
Case 8: 65yo with 30 minutes of chest pain. AVSS. Old then new ECG
Case 9: 50yo with pleuritic chest pain. AVSS. Old then new ECG:
Case 10: 70yo VF arrest. ECG pre-arrest and then post-ROSC
ST ELEVATIONS mnemonic and Occlusion MI
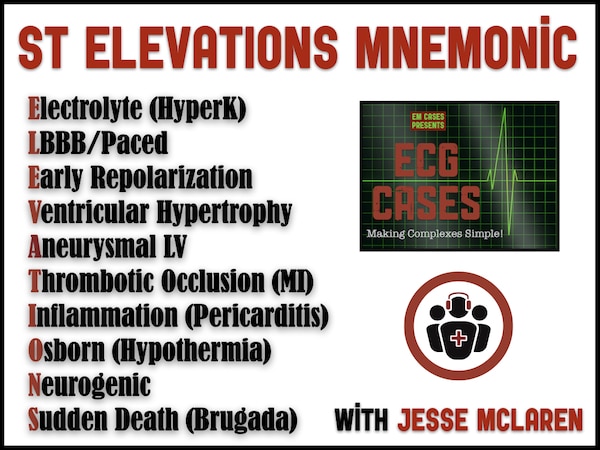
Most patients presenting to the ED with chest pain and ST elevation don’t have acute thrombotic occlusion [1]. The differential of ST elevation includes hyperkalemia, baseline conduction (LBBB, early repolarization), structural changes (LVH, LV aneurysm), acute ischemia or inflammation (including occlusion mimics discovered on angiography, like coronary vasospasm, myocarditis or takotsubo), and miscellaneous rarer causes. These can be remembered by the mnemonic “ELEVATIONS”:
- Electrolyte (hyperkalemia)
- LBBB/ventricular paced
- Early repolarization
- Ventricular hypertrophy
- Aneurysmal LV
- Thrombotic occlusion (OMI)
- Inflammation (pericarditis)
- Osborn wave (hypothermia)
- Neurogenic (eg SAH, ICP)
- Sudden death (Brugada)
These all have ST elevation and are not mutually exclusive (eg, hyperkalemia or ischemia can induce the Brugada phenocopy, or patients with LBBB or LVH can develop thrombotic occlusion). As a result, only looking at the ST segment and dichotomizing it by millimeter criteria doesn’t differentiate between different causes of ST elevation (eg early repolarization, pericarditis, thrombotic occlusion), and doesn’t identify acute occlusion in the presence of chronic ST elevation (eg from LBBB, LVH or LV aneurysm). These limits of the STEMI paradigm were identified early on, as the National Heart Attack Alert Program Coordinating Committee explained in 1994: “ECG abnormalities may be subtle or open to different interpretation, such as early repolarization or pericarditis. Only borderline or minimal ST-segment elevation may be present, and the emergency physician may be uncertain of its significance. The presence of left bundle branch block or left ventricular hypertrophy may complicate ECG diagnosis. The emergency physician may suspect that the ST elevation is old, but a previous ECG may be unavailable for comparison. The computer interpretation of the ECG on which some physicians rely may be incorrect.” [2] At the time little could be done to address these limitations, beyond other false dichotomies—for example that concave ST elevation differentiates benign causes (eg pericarditis or early repolarization) from occlusion, or that Q waves distinguish old from new MI. The STEMI paradigm was further reinforced by a definition that excludes LBBB and LVH and that excludes minimal ST elevation as “Non-STEMI”. As a consequence, the STEMI paradigm misses 25% of acute coronary occlusions that don’t meet criteria[3], and can result in unnecessary cath lab activation for ST elevation not caused by acute occlusion.
But over the past 25 years later, there have been major advances in ECG interpretation that have addressed many of the earlier limitations. While computer interpretation is still notoriously inaccurate, there are many useful decision rules that can help[4]. While 40% of LAD occlusion present with concave and borderline ST elevation, there is a rule for differentiating early repolarization from LAD occlusion—not just based on magnitude and morphology of ST elevation, but also Q waves, terminal QRS distortion, ST depression, T wave inversion, reciprocal changes, and a formula for subtle cases[5]. While STEMI criteria has poor sensitivity for inferior MI, reciprocal ST depression in aVL is much better at identifying subtle inferior MI and differentiating MI from pericarditis. [6]. While Q waves can develop within an hour of occlusion, the ratio of T waves to QRS complex can distinguish anterior STEMI from old LV aneurysm morphology. [7] While LVH continues to complicate the diagnosis of acute coronary occlusion, the modified Sgarbossa criteria can identify occlusion in the presence of LBBB.[8].
A paradigm shift from STEMI to Occlusion MI (OMI) would benefit both those currently diagnosed as “STEMI” and those currently diagnosed as “NSTEMI”. A quarter of Code STEMI patients with culprit lesions have STEMI-equivalents or subtle occlusion on their first ECG that don’t meet STEMI criteria and that are associated with prolonged ECG-to-Activation time, which would benefit from earlier recognition[9]. And a quarter of patients admitted as “NSTEMI” can be reclassified as Occlusion MI based on advanced ECG interpretation (eg minor STE with reciprocal STD, or hyperacute T waves), and this STEMI(-)OMI(+) subgroup has a higher mortality rate that would benefit from earlier reperfusion. [10]
Back to the cases
Case 1: hyperkalemia
- Heart rate/rhythm: NSR
- Electrical conduction: prolonged PR/QRS, LAFB
- Axis: left
- R-wave: delayed R wave progression
- Tension: no hypertrophy
- St/T: mild anterior concave STE and diffuse narrow/peaked T waves
Impression: multiple findings of hyperkalemia. Treated empirically with calcium, insulin/dextrose, and dialysis. Potassium level 9.0. Post-dialysis ECG had resolution of conduction delays, ST elevation and peaked T waves:
Case 2: LBBB
- H: sinus brady
- E: LBBB
- A: left axis
- R: normal R wave progression
- T: can’t assess LVH
- S: discordant anterior STE, in V2 STE/S = 5/47 = 0.11
Impression: LBBB without evidence of OMI. Though this meets the original Sgarbossa criteria of 5mm STE and could have resulted in unnecessary cath lab activation, it was recognized to be proportional to large voltage and does not meet modified Sgarbossa criteria. Patient hemodynamically stable, admitted for CHF, ruled out for MI.
Case 3: LBBB + occlusion, STEMI(-)OMI(+)
- H: sinus tach
- E: LBBB
- A: normal axis
- R: delayed R wave progression
- T: can’t assess LVH
- S: appropriate discordant STE in V1 (3/17=0.18), but concordant STD in V3 (meeting original Sgarbossa criteria) and disproportionate STD in I/II/aVF and V4-6 (STD/R>0.30) meeting modified Sgarbossa criteria
Impression: LBBB with OMI (both on ECG and clinically concerning with diaphoresis and borderline hemodynamics), not initially recognized. ECG-to-Activation time 125 minutes. Cath lab activated: 90% left main stenosis, then cardiac arrest.
Case 4: early repolarization
- H: sinus brady
- E: normal conduction, incidental U wave V1-3
- A: normal axis
- R: normal R wave progression
- T: (LVH criteria not applicable <35yo)
- S: concave STE and T wave proportional to large QRS, with J wave V3-4. There is a tiny Q in V4 but not V2-3. There are no convex ST segments, no STE>5mm, no terminal QRS distortion (V3 has no S wave but it has a J wave), no ST depression, no T wave inversion and no reciprocal changes
Impression: early repolarization without evidence of OMI. Meets STEMI criteria with 3mm STE in V1-3 but the Smith formula gives a value of 10.3 which is highly likely to be early repolarization. Patient had a similar prior ECG, negative troponins and was well on follow up.
Case 5: LAD occlusion, STEMI(-)OMI(+)
- H: NSR
- E: normal conduction
- A: normal axis
- R: reverse R wave progression, V2-3, small Q in V2-3 and inferiorly
- T: no hypertrophy
- S: mild concave and inferior STE, terminal QRS distortion in V2 (no S or J wave), hyperacute T wave V1-3 (as large as the QRS in V2 and larger than the QRS in V3)
Impression: does not meet STEMI criteria but has multiple signs of OMI, and the Smith formula gives a value of 20.4 which is likely LAD occlusion. Delayed diagnosis (ECG-to-Activation time 55 minutes) until first troponin I came back at 1000. Wrap-around LAD occlusion (producing anterior and inferior STE) with 100% occlusion mid-vessel, peak troponin 50,000. Discharge ECG: reperfusion T wave inversion anterior and inferior:
Case 6: LVH + LAD occlusion, STEMI(-)OMI(+)
- H: NSR
- E: normal conduction
- A: normal axis
- R: normal R wave progression, large voltage
- T: LVH
- S: anterior STE (convex in V1 and concave V2-4) and hyperacute T wave in V3 (greater than the entire QRS complex)
Impression: LVH could produce the anterior STE and is excluded from STEMI criteria, but the hyperacute T wave in V3 is massive and disproportionate to its normal sized QRS complex. Rapidly diagnosed (ECG-to-Activation time 10 minutes): 99% mid LAD occlusion, trop I peak at 38,000. Discharge ECG revealed reperfusion T wave inversion:
Case 7: Q wave from subacute LAD occlusion, STEMI(+)OMI(+)
- H: NSR
- E: normal conduction
- A: normal axis
- R: anterior loss of R waves with QS in V1-3 and QR in V4
- T: no hypertrophy
- S: nonconcave STE V2-4 with hyperacute T waves, T/QRS in V3 = 5/8 = 0.63
Impression: with anterior QRS waves and one lead with T/QRS>0.36 this is either an old MI with acute occlusion, or all from an acute occlusion. The patient had no history of MI and hours of acute chest pain which produced a Q wave, but still had hyperacute T waves. Rapidly diagnosed (ECG-to-Activation time 8 minutes): 99% mid LAD occlusion, first trop I was 43,000 and peak was >50,000. Discharge ECG had ongoing anterior QS waves with mild STE but no longer hyperacute T waves: but V2 has T wave inversion and V3 has T/QRS = 2/10 = 0.20.
Case 8: subtle inferior MI, STEMI(-)OMI(+)
- H: NSR
- E: first degree AV block
- A: normal axis
- R: normal R wave progression
- T: no hypertrophy
- S: mild inferior concave STE with hyperacute T wave, reciprocal STD/TWI in aVL, and ST pseudonormalization in V2
Impression: doesn’t meet STEMI criteria, but the new reciprocal change in aVL makes the inferior STE and hyperacute T waves diagnostic of inferior OMI. Repeat ECG had similar changes and patient had ongoing chest pain so cath lab activated (ECG-to-Activation time 22 minutes): 100% mid RCA occlusion, trop I rose from 25 to 50,000. Discharge ECG: reperfusion T wave inversion inferiorly and posterior (giving appearance of hyperacute T wave in V2):
Case 9: pericarditis
- H: NSR
- E: normal conduction
- A: normal axis
- R: normal R wave progression
- T: no hypertrophy
- S: mild inferolateral concave STE, PR depression, without hyperacute T waves or reciprocal change in aVL
Impression: while this meets STEMI criteria of 1mm STE in two contiguous leads, what’s most reassuring is not the mild degree or concave morphology of the ST segments, but the lack of reciprocal change in aVL. However, this patient had a full workup to exclude other causes besides pericarditis: serial ECG and troponins were negative, echo was normal, D-dimer was positive but CTPA ruled out PE. Patient was given a discharge diagnosis of pericarditis, treated with ASA and colchicine, and had normalization of ST changes:
Case 10: Brugada syndrome
- H: NSR pre-arrest and AF post-arrest
- E: RBBB
- A: normal axis
- R: tall R’ in V1
- T: no hypertrophy
- S: coved STE with TWI in V1; diffuse ST depression post-arrest
Impression: Brugada syndrome with VF arrest. Post-ROSC diffuse ST depression normalized, patient had normal cath, and discharged after ICD placement
Take home points for ST ELEVATIONS mnemonic and Occlusion MI
- Consider the differential for ST “ELEVATIONS”: Electrolyte (hyperK), LBBB/paced, Early repolarization, Ventricular hypertrophy, Aneurysmal LV, Thrombotic occlusion, Inflammation, Osborn waves, Neurogenic, Sudden death (Brugada)
- Rules for occlusion can help differentiate early repolarization from LAD occlusion, subtle inferior MI from pericarditis, anterior STEMI from LV aneurysm, and occlusion MI in the presence of LBBB.
References for ECG Cases 17 ST ELEVATIONS mnemonic and Occlusion MI
- Brady WJ, Perron AD, Martin ML, et al. Cause of ST segment abnormality in ED chest pain patients. Am J of Emerg Med 2001 Jan;19(1):25-28
- National Heart Attack Alert Program Coordinating Committee, 60 Minutes to Treatment Working Group: Emergency department: Rapid identification and treatment of patients with acute myocardial infarction. Ann Emerg Med Feb 1994;23:311-329
- Khan AR, Golwala H, Tripathi A, et al. Impact of total occlusion of culprit artery in acute non-ST elevation myocardial infarction: a aystematic review and meta-analysis. Eur Heart J 2017;38:3082-9
- Miranda DF, Lobo AS, Walsh B, et al. New insights into the use of the 12-lead electrocardiogram for diagnosing acute myocardial infarction in the emergency department. Can J Cardiol 2018 Feb;34(2): 132-145
- Driver BE, Khalil A, Henry T, Kazmi F, Adil A, Smith SW. A new 4-variable formula to differentiate normal variant ST segment elevation in V2-V4 (early repolarization) from subtle left anterior descending coronary occlusion – Adding QRS amplitude of V2 improves the model. J Electrocardiol. 2017;50(5):561-569
- Bischof J, Worral C, Thompson P, et al. ST depression in lead aVL differentiates inferior ST elevation myocardial infarction from pericarditis”. Am J Emerg Med. 2015;34(2):149-154
- Klein LR, Shroff GR, Beeman W, et al. Electrocardiographic criteria to differentiate acute anterior ST-elevation myocardial infarction from left ventricular aneurysm. Am J of Emerg Med 2015;33:786-790
- Meyers HP, Limkakeng AT, Jaffa EJ, et al. Validation of the modified Sgarbossa criteria for acute coronary occlusion in the setting of left bundle branch block: a retrospective case-control study. Am Heart J 2015 Dec;170(6):1255-64
- McLaren JTT, Kapoor M, Yi SJ, et al. Using ECG-to-Activation time to assess emergency physicians’ diagnostic time for acute coronary occlusion. J Emerg Med 2020 Oct 12; S0736-4679(20)30964-1
- Aslanger EK, Yıldırımtürk Ö, Şimşek B, et al. DIagnostic accuracy oF electrocardiogram for acute coronary OCClUsion resuLTing in myocardial infarction (DIFOCCULT Study). IJC Heart Vasc 2020 Oct;30: 100603























Leave A Comment