Episode 31: LP, Spontaneous Pneumothorax and Ultrasound Guided Fracture Reduction
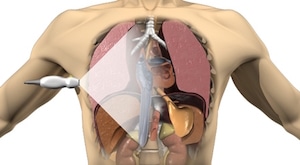
In this episode, Dr. Jordan Chenkin & Dr. Jamie Blicker discuss positioning, landmarking, and best technique for lumbar puncture, how to minimize post-LP headache and traumatic taps, as well as when CT head is not required prior to LP. They discuss the indications, contraindications, trouble-shooting and pros and cons of needle aspiration, small bore pleural catheter with Heimlich valve and large bore chest tube for the treatment of spontaneous pneumothorax. Dr. Chenkin presents an intriguing argument for why he uses ultrasound-guided fracture reduction routinely in the ED, and we end with a few tips and tricks using skin adhesive for some unorthodox indications.