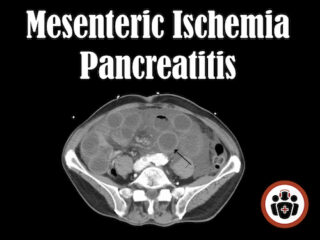
Episode 42: Mesenteric Ischemia and Pancreatitis
In this episode Dr. Steinhart, (one of my biggest mentors – the doc that everyone turns to when no one can figure out what’s going on with a patient in the ED), & Dr. Dave Dushenski, (a master of quality assurance and data analysis, who would give David Newman a run for his money), discuss the 4 diagnoses that make up the deadly & difficult diagnosis of Mesenteric Ischemia, it’s key historical and physical exam features, the value of serum lactate, D-dimer & blood gas, when CT can be misleading, ED management of Mesenteric Ischemia, the difficult post-ERCP abdominal pain patient, the pitfalls in management of Pancreatitis, the BISAP score for Pancreatitis compared to the APACHE ll & Ranson Score, the comparative value of amylase and lipase, ultrasound vs CT for pancreatitis and much more…